Study: Oral Antibiotics Could Be Responsible For Dramatic Increase Of Kidney Stones
Follow CBSPHILLY Facebook | Twitter
PHILADELPHIA (CBS) – A groundbreaking new study is the first to link the use of antibiotics to kidney stones.
Emma Gaal is part of the epidemic of young people, especially girls, who develop kidney stones. There's been a 70 percent increase over the past 30 years.
Research: Third-Hand Smoke Spreads Indoors
"Everyone thinks you're older when you get them, so no one believed it when I said I had kidney stones," said Gaal.
Oral antibiotics could be responsible for the dramatic increase of kidney stones, according to a new study that covered 13 million people.
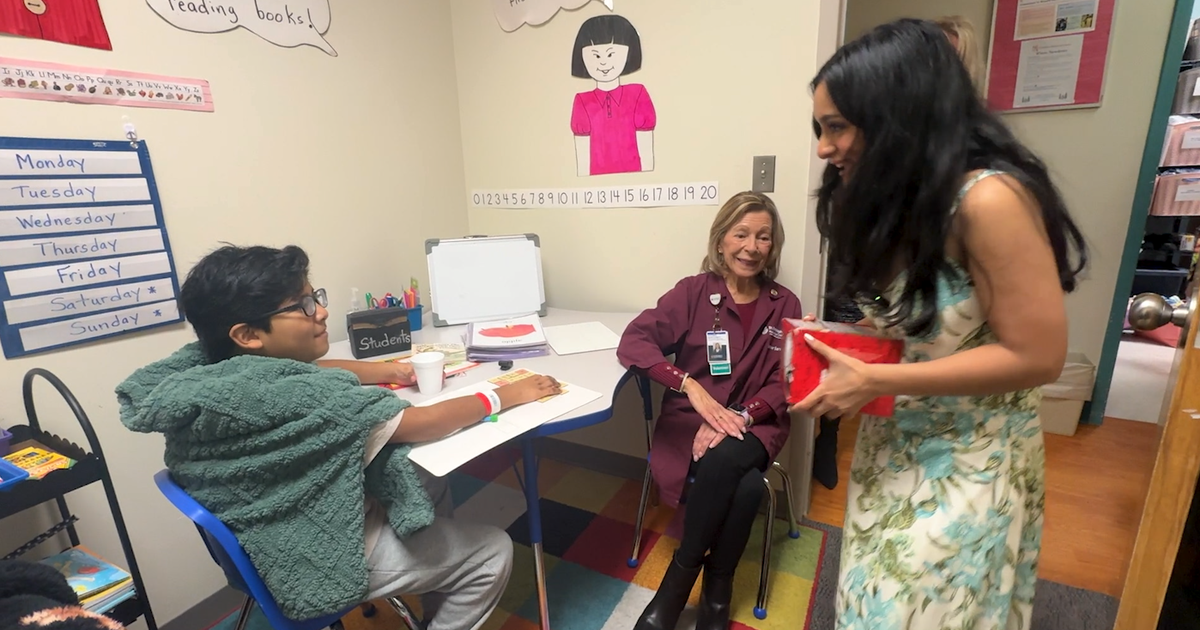
"For some medications, the risk was about 50 percent increase. For other medication, it was about a two times greater increase, so there was a lot of variation depending on the antibiotic class," said Dr. Gregory Tasian, who led the research at Children's Hospital of Philadelphia.
He's the first who links antibiotics to kidney stones.
"Sulfa drugs include medications like Septer or Bactrim. Some of the other antibiotic classes include fluoroquinolones, which would be something like ciprofloxacin or levofloxacin and Levaquin," said Tasian.
He says the theory is that antibiotics disrupt healthy bacteria in the intestinal or urinary tract which then leads to the formation of kidney stones.
"Antibiotics have saved lives. They are important to use for clinically indicated infections, but we also know that antibiotics are often prescribed unnecessarily," said Tasian.
It's estimated that about 30 percent of antibiotic prescriptions are inappropriate. The research showed the earlier they're used, the higher the risk for stones.
CDC 'Ticks' Off Twitter With Photo Of Poppyseed Muffin With Ticks
"I think this is the tip of the iceberg," Tasian says.
For Emma, drinking lots of water helps keep the kidney stones from coming back--a fear she now lives with.
"Whenever I get a pain in the stomach, I think, 'Oh God, kidney stones again,'" she says.
Kidney stones are not only painful, they also increase the risk for fragile bones, hypertension and heart disease.
Now that the link has been established between antibiotics and stones, researchers will next look for a cause, then ways to better treat or even prevent them.
Dr. Tasian's findings will appear in an upcoming issue of the Journal of the American Society of Nephrology (JASN).
For their study, the investigators determined the association between 12 classes of oral antibiotics and nephrolithiasis in a population-based study within 641 general practices providing electronic health record data for more than a 13 million children and adults from 1994 to 2015 in the United Kingdom. The team matched 25,981 patients with nephrolithiasis to 259,797 controls by age, sex, and practice at the date of diagnosis (termed the index date).
Exposure to any one of five different antibiotic classes three to 12 months before the index date was associated with nephrolithiasis. Risks were increased 2.3 times, 1.9 times, 1.7 times, 1.7 times, and 1.3-times for sulfas, cephalosporins, fluoroquinolones, nitrofurantoin/methenamine, and broad-spectrum penicillins, respectively. The risk of nephrolithiasis decreased over time, but it remained elevated at 3-5 years after the antibiotic prescription. Also, the risk was greatest for exposures at younger ages. Previous research has shown that children receive more antibiotics than any other age group, and 30 percent of antibiotics prescribed during ambulatory care visits are inappropriate.