New Study Examines Health Effects Of Inducing Labor For Pregnant Women
Follow KDKA-TV: Facebook | Twitter
PITTSBURGH (KDKA) -- Morgan Webb just had her first baby. Her pregnancy was full of excitement.
"It was a great shock to find out we were expecting Emerson," Morgan says, "but I had a great pregnancy."
Labor was induced at 39 weeks because of a study she agreed to be in. It included more than 6,000 healthy women in their first pregnancy at 41 hospitals across the United States, including Magee-Womens Hospital. They were randomly assigned to be induced or not.
When she found out she would be induced, it made her a little nervous.
"I had a lot of concerns because I didn't want to mess with my body. I didn't want to mess with Mother Nature," Morgan continues. "I wanted it just to happen. I wanted to experience everything by itself."
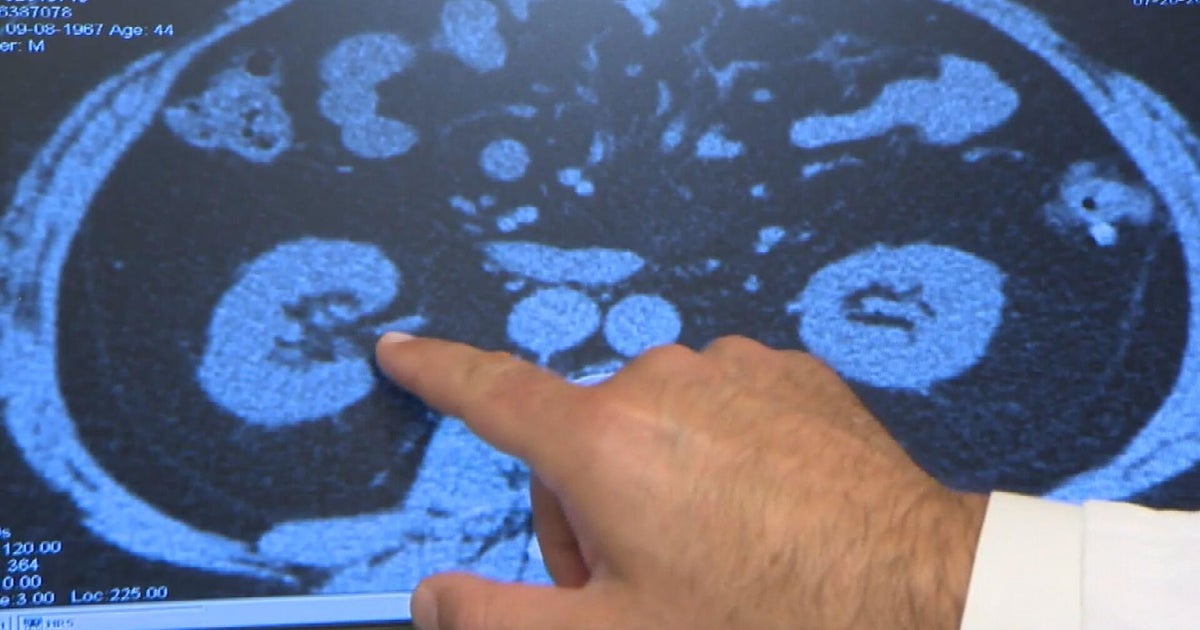
Induction is a process of bringing on labor in an expectant mom who is not in labor. Doctors can break the water sac around the baby, and use medicines to soften the opening of the womb and to cause contractions. Doctors wanted to see if there was a difference in outcomes if labor was induced at 39 weeks, or if labor occurred on its own.
"The point of kind of maximal maturity for a baby is at 39 weeks of gestation, which is why that was selected," says Magee-Womens Hospital Maternal Fetal Medicine specialist Dr. Hyagriv Simhan.
Turns out, the induction group saw some benefits.
"In that induction group, we saw a lower risk of cesarean section, we saw a lower risk of developing hypertensive disorders of pregnancy, preeclampsia, and we saw that their babies were less likely to require neonatal respiratory support," says Dr. Simhan.
In general, about one in four women have labor induced -- either for medical reasons, such as high blood pressure, high blood sugar, or going beyond the due date, which carries a higher risk of stillbirth -- or for convenience and predictability, which can be important for a family's schedule.
Could this study influence the management of late pregnancy? Perhaps.
The study was presented at the Society of Maternal Fetal Medicine Annual Meeting, and it still has to be peer reviewed and published.
Questions came up about the costs of more inductions versus the savings of fewer C-sections, and about how induction was carried out.
"In this study, we didn't pre-specify how the induction of labor would take place. It varied as it would vary across 41 hospitals in the U.S., each of which has its own particular protocols and approaches," Dr. Simhan explains.
Morgan's induction went smoothly, and in the end, she was glad she was in that group, though not everyone shares her enthusiasm.
"So, a lot of people are just like, 'I don't know, I don't agree that you did it,'" says Morgan, "I said, 'Well, there's no problems with her, she's great!"