Dementia Wards In Pennsylvania Hit Hard By COVID-19 Pandemic
PITTSBURGH (AP) — In the weeks before she died of COVID-19 in the dementia unit of a suburban Philadelphia personal care home, Barbara Demech often lamented about the Alzheimer's disease that began gripping her mind a decade earlier.
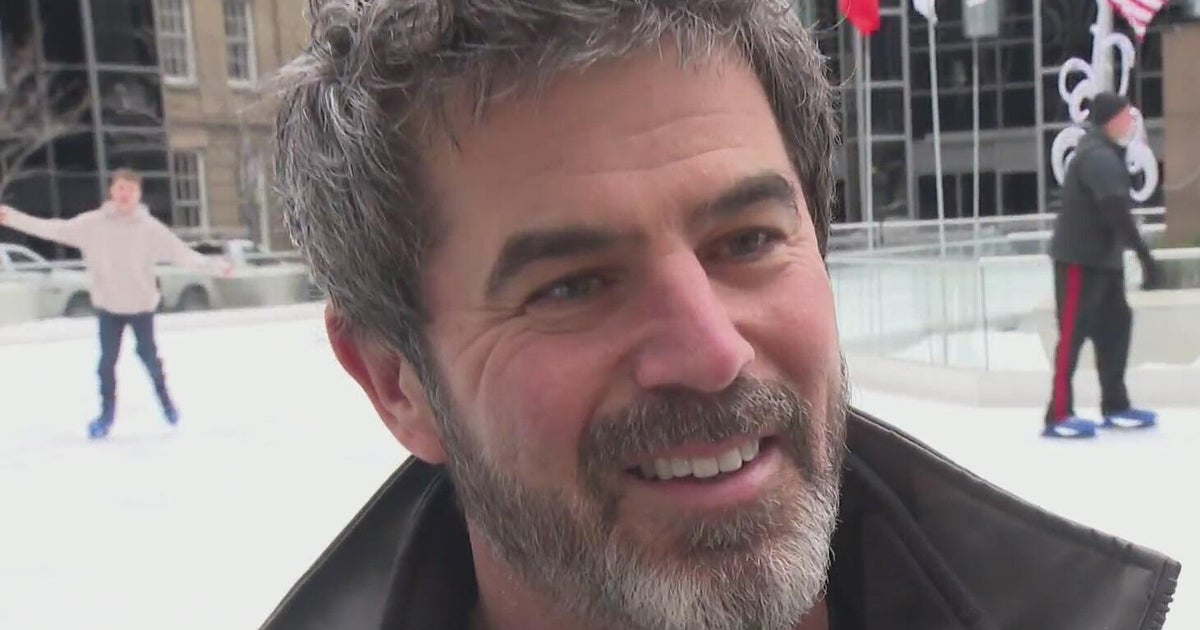
"She'd say to me, 'I just feel like somebody is in there taking over,'" recalled her son, Mike Demech. "She would say it often toward the end."
Like so many people in the throes of dementia, it was difficult for her and others in the "memory care" unit to take the most basic steps — like wearing a mask or social distancing — and prevent themselves from contracting the disease.
By the time the virus raged through The Birches at Newtown — starting in her unit a year ago — 26 residents had died, including Mrs. Demech, in the second deadliest outbreak of any personal care home in the state.
The deaths in the home and many others across Pennsylvania highlight the dangers that residents with dementia faced during the pandemic and a state oversight system that imposed few protections during the worst of the crisis.
Less than a third of all personal care homes and assisted living facilities in the state have dementia units — 343 in all. And yet the special subset of homes with those units account for nearly 70% of all such facilities that had five or more deaths from the virus, the Pittsburgh Post-Gazette found.
The risks with dementia residents in personal care homes and assisted living facilities — which are far less regulated than nursing facilities — brought yet another set of problems for public health officials that they had never confronted.
"You're going to try to tell these folks to wear a mask?" asked Mr. Demech, whose mother died last May at 80. "It's not that they wouldn't want to comply. It's just that they don't have the mental capacity to follow A,B, C or D." Officials at Birches did not return calls for comment.
The disease took a devastating toll on long-term care homes, but the impact on people suffering from dementia represents one of the least known problems in long-term care homes during the pandemic.
A lack of training and staffing requirements by the state and as well as a failure to ensure homes are complying with minimal requirements left many of the state's most vulnerable residents without critical protections, say experts.
Dementia patients dying
Just keeping the infections from dementia wards has been daunting, said Dr. David Nace, chief medical officer for UPMC Senior Communities and co-lead of the state's regional collaborative that responds to outbreaks in long-term care homes in Western Pennsylvania.
"It would spread among the (dementia) residents very quickly, he said, citing a host of reasons, including "the inability to maintain hand hygiene, social isolation, masking, cough etiquette, all of those things." In the eight counties in southwest Pennsylvania, 17 of the 34 personal care and assisted living homes with five or more deaths from the virus had dementia wards.
Kevin Cysyk, director of assisted living and personal care for the Pennsylvania Health Care Association, said that data could be misleading because dementia units tend to be in the larger homes, and those homes are more likely to have more deaths.
However, a national study released in February that reviewed more than 60 million medical records found people with dementia — living in long-term care facilities or not — were twice as likely as those without dementia to be infected with the virus and nearly four times as likely to die from it.
Dr. Pamela Davis, a co-author of that peer-reviewed study in Alzheimer's & Dementia: The Journal of the Alzheimer's Association, said residents living in memory wards were at a clear disadvantage when it came to fending off the virus.
"It's the dementia units that are kind of leading the way both in infections and consequences," said Dr. Davis, dean emerita of the School of Medicine at Case Western Reserve University.
Dr. Davis said further studies will examine the reasons for the higher rates, including whether damage to the blood-brain barrier that occurs in people with dementia makes it easier for the virus to enter the brain and cause significant damage.
'It really spread'
At The Sheridan at Bethel Park, the virus started in the memory care unit, said Wendy Mildner, the administrator, and eventually spread to 56 of the 97 residents — including most of the people in the memory unit. Seven of those residents later died.
"Once it got into memory care, it really spread," she said. "In memory care, it was really difficult to get them to wear masks or social distance."
Part of the problem in personal care homes is they were initially created in the state to serve as retirement homes for people who were mobile and in relatively good health. As the homes evolved -- and the elderly population boomed — more people with poor health conditions began moving into the facilities, including those with dementia.
But unlike the oversight of nursing homes, state regulations didn't keep up with the growth. For instance, there are no state infection control regulations for personal care homes — critical to helping stave off something like COVID-19.
Personal care homes are also not required to have medically trained staff as a nurse on site.
Even for those who are on staff, a home with a dementia ward must only provide two hours of care a day to each resident as opposed to one hour for residents without dementia.
But adding more workers is easier said than done, said Zach Shamberg, president and CEO of the Pennsylvania Health Care Association, which represents many of the state's long-term care homes.
"We're struggling to find workers to fill the positions now," said Mr. Shamberg. "And anything that we do, or anything that we want to do, is really going to have to be a collaborative effort to make sure we have that pipeline" of workers to fill any boost in staffing requirements.
Bracing for more
Adding to the problem of a worker shortage is that people are living longer and the number of people diagnosed with dementia will grow by about 14% by 2025, according to the Alzheimer's Association.
"Dementia is the next explosion in our senior population," said Mr. Shamberg, who noted that his grandfather has dementia and is in a personal care home.
State data shows that's the case: The number of personal care and assisted living homes with dementia units in Pennsylvania has increased by 76 — or 22% — since 2015.
Some believe the growth in demand for dementia care will only increase because of the pandemic, largely from the isolation that many seniors experienced either living at home or in long-term care facilities.
"Unfortunately the increase for the need of (dementia care) has just gone through the roof over the last year," said Cathy Himes, administrator at Grace Manor at North Park personal care home, which opened a new, 18-bed dementia unit in February in the midst of the pandemic.
That was true for Mike Majcher's mother, Frances Majcher, 95, who lived in Sunrise of McCandless personal care home's dementia unit before she was infected with COVID-19 and died on January 3.
"For a long time they tried to do activity carts and feed them in their rooms to isolate them and try to keep them safe," said Mr. Majcher of McCandless. "But they found the isolation was making their dementia worse, even with activities or meals in their room."
Eventually, though, the virus swept through the memory unit and the rest of the home, infecting 35 residents and killing 17 —. one of the 10 deadliest outbreaks among personal care and assisted living homes in the state. Sunrise officials would not answer questions about the outbreak.
Lack of critical training
Beyond the staffing levels, experts said the state does not require nearly enough training to care for people now filling the homes' dementia wards.
Staff members who work with dementia residents in assisted living homes need only eight hours of training when they are hired and an additional eight hours annually. Personal care home staff must have just six hours of yearly training, but the curriculum is largely decided by the home and is not standardized.
Teepa Snow, an expert on dementia care who provides training to homes through her company, Positive Approach to Care, said in many states like Pennsylvania, there are no regulations dictating the proper training for the staffs, and "the most many (homes) do for training is to have them watch a video for six hours, and then you're ready to go."
On top of that, the state's small number of inspectors rarely cite a home for failure to provide enough daily care to any residents, although it does regularly cite them for failing to staff enough people for night shifts to perform fire drills.
"They're more concerned about the fire drill than actual care," said Ms. Snow. "The amount of care and the amount of support is not monitored" by the state.
The state does mandate that both types of homes offer weekly programs in dementia units for gross motor activities and exercise; self-care; social activities; social and memory enhancement exercises, and outdoor activities.
While Dr. Nace said "staffing clearly plays a role" in helping to prevent outbreaks — something his staff saw play out in the homes they responded to — but how much required care is actually provided is unclear. And whether each facility actually meets the two hours of daily care requirement is unclear as well.
Unlike nursing homes, which are overseen by federal and state requirements that require staffing levels be disclosed, there is no similar system of assessing the care provided at personal care or assisted living homes in Pennsylvania.
The Pennsylvania Department of Human Services, which oversees personal care and assisted living homes, said in an emailed response to questions that it was "aware" of the impact of COVID-19 on residents with dementia in the homes.
In its guidance to long-term care homes early in the pandemic, DHS did note that having a dementia unit "may make a facility more prone to outbreaks" and that they should have more regular screening and testing of residents to root out infections quickly.
Although DHS did not have figures on the number of residents with dementia who became infected or died, it said that out of the 600 rapid responses to outbreaks conducted by the regional collaboratives, 73 were to facilities with dementia wards.
'What went wrong'
State Rep. Frank Farry, R-Bucks, chair of the state House Human Services Committee that oversees personal care and assisted living regulations, said he didn't know about the connection between dementia, long-term care, and the virus until the Post-Gazette described the data it found.
He was concerned to learn about the criticism of the state's staffing and training requirements, as well as the lack of requirement for medical staff in personal care homes, especially in dementia units.
"I'd like to talk to all the stakeholders and find out the root of those regulations from the providers as well as the department," he said. "Because just looking at it, it doesn't seem like it's sufficient, whether it's not having health care providers on-site, as well as the amount of care provided."
Despite the problem of dementia and virus cases in the homes in Pennsylvania, Sen. Judy Ward, R-Blair, chair of the state Senate's Youth and Aging Committee — which has held multiple hearings about how to respond to the pandemic in long term care — said dementia's role "has not come up" in any hearing so far.
"I was shocked to hear" the Post-Gazette's data on the link between dementia units and COVID-19 deaths, said Ms. Ward, who wants to look closer at the problem.
"I really am committed to looking at what went wrong and how we can make it better," Ms. Ward said.
Sara Murphy, vice president of programming and services for the Alzheimer's Association of Greater Pittsburgh, said her group is pushing hard to make changes to the state's regulations for dementia units.
"It's 100% on our radar because it's not up to par by any means," Ms. Murphy said. "We're working with the department to provide clear recommendations for changes, including standardization of training" for staff who work with residents with dementia.
Last summer, as the pandemic grew, the Alzheimer's Association made a series of recommendations to the state to change the state's long-term care regulations, including improving training, said Jen Ebersole, director of state government affairs for the Alzheimer's Association in Pennsylvania.
"We are taking a look at how these regulations can be changed," Ms. Ebersole said. "We're already in a problem area, and it's only going to get worse if we don't make changes."
(Copyright 2021 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.)