Busted! 8 mammogram truths every woman must know
Do mammograms save lives? Of course they do. But is mammography the surefire "fix" for the breast cancer problem that many women believe it to be? Unfortunately not, says Dr. Laura Esserman, director of the Carol Franc Buck Breast Care Center at the University of California at San Francisco.
In fact, she says, there are quite a few "inconvenient truths" about mammography that women should be aware of. Here are six.
Note: This slideshow is not medical advice. If you have any concerns about breast cancer, talk to your doctor.
Self-Awareness Matters
No matter what mammogram schedule women follow, they should be on the lookout for any changes in their breasts that suggest trouble. Fact is, says Dr. Esserman, half of all breast cancer patients spot their own tumors by checking their breasts.
Mammography "is not a substitute for being aware of your body," says Dr. Esserman.
Mammos Can Lead to Medical Problems
When a mammogram shows something "suspicious," the woman is typically asked to follow up with additional scans and, in many cases, biopsies. Yet up to 80 percent of biopsies come back negative, meaning that there is no cancer.
Biopsies are painful, and some result in infection. And then there is the enormous stress women experience during the time they think they might have cancer.
Dr. Esserman says that any woman told she needs a breast biopsy should ask the doctor whether it might be possible to "watch and wait" the suspicious breast rather than have an immediate biopsy.
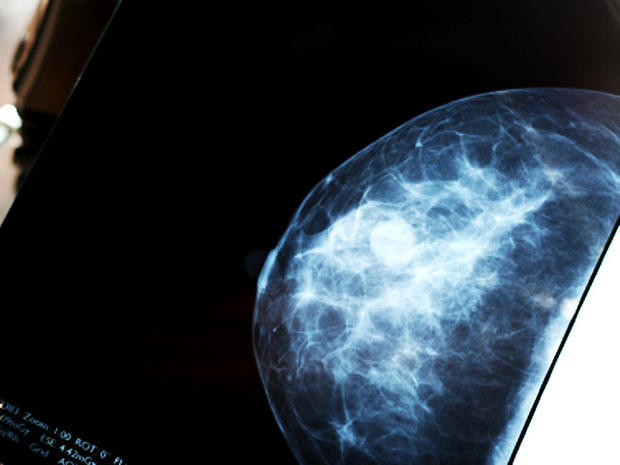
Age Makes a Difference
The breasts of younger women - those in their forties or below - tend to be dense, and mammograms aren't particularly effective at spotting cancer in dense breasts. For these women, mammography is more likely to result in being called back for a biopsy even when no cancer is present.
On the other hand, women age 75 or older tend to have slower-growing tumors, so mammography might not make much sense for them.
Women in these age groups should talk with their doctor about the value of mammography, says Dr. Esserman.
Screening Guidelines Can Be Confusing
Experts disagree about screening guidelines. The American Cancer Society says women should get regular mammograms starting at age 40. But last November, the U.S. Preventive Services Task Force caused a firestorm of controversy when it revised its screening recommendations, saying that women without personal risk factors should have their first mammogram at age 50 and then every 18 to 24 months after that.
In addition, the task force said women in their forties and over age 74 should make their decision about mammography on an individual basis, after speaking with their doctor.
So what's a woman to do? Know your body, your family history of breast cancer, and your own personal risk factors, says Dr. Esserman. Then talk to your doctor.
Mammos Can Miss Aggressive Tumors
Some women seem to think that as long as they get regular mammograms, they'll be safe from breast cancer. That's not necessarily so. Some cancers grow so quickly that they develop between scheduled mammograms. These can be especially dangerous.
Increased use of mammography has resulted in more tumors being found, but many of these are slow-growing, relatively benign cancers. Says Dr. Esserman, "We are not going to screen ourselves into a cure." To do better, she says, doctors need to find smarter ways of screening and to develop more effective treatments for aggressive cancers.
Mammgrams Have to Be "Read"
The results of a mammogram don't just jump out. A mammogram has to be "read" by a skilled radiologist - ideally one who has lots of experience.
One way women can help ensure they're getting reliable mammography results is to go to a mammography center where each "reader" sees about 2,000 mammograms a year, according to Dr. Esserman. And, she says, it's best to go to a center that specializes in breast imaging rather than to a general radiology center.
Prevention Counts
For women who are at high risk for breast cancer, regular mammography may be less important than taking steps to reduce the risk. Dr. Esserman says women should know their family history of cancer and t heir personal risk factors in order to make sound decisions about the value of mammography. (Smoking, drinking, and being overweight are three things that increase a woman's risk for breast cancer.)
Should I or Shouldn't I?
With conflicting guidelines, it's not easy to know when is the right time to get a mammogram.
Dr. Esserman says it's vital that every woman knows her body, her family history of breast cancer, and her own personal risk factors.
Then talk to her doctor.