Should the CDC cut the 5-day COVID-19 isolation guidelines? Experts weigh in.
The Centers for Disease Control and Prevention is weighing its first major revision to COVID-19 guidance since the end of the federal public health emergency last year.
Among the changes being considered by the agency is an end to its pandemic-era plea that people isolate for at least five days after testing positive for COVID-19, according to a Tuesday report by The Washington Post.
Instead, Americans who test positive for COVID-19 could reportedly stop isolating and potentially return to work and other activities once their fever ends for at least 24 hours and their symptoms are mild and improving. Such guidelines would be similar to recommendations announced by state health authorities in Oregon last year.
Current CDC guidance has said since 2021 that people with COVID should isolate for at least five days, regardless of symptoms. That is different from the CDC's guidance for other common respiratory viruses, influenza and RSV, or respiratory syncytial virus.
A spokesperson for the CDC declined to confirm whether the agency was planning this change.
"No updates to COVID guidelines to announce at this time. We will continue to make decisions based on the best evidence and science to keep communities healthy and safe," CDC spokesperson David Daigle said in a statement.
The current five-day isolation guidance had already been a compromise between the science of how to curb the spread of the virus and other priorities, Dr. Céline Gounder, a CBS News medical contributor and editor-at-large for public health at KFF Health News, told "CBS Mornings" on Wednesday.
"I think this is really an effort on the part of the CDC to align their guidance with what people are willing and able to do. People have not been following this guidance, let's be real," Gounder said.
Gounder said COVID-19 isolation policies had taken a toll on many who lost wages or had to pay extra for child care, as officials tried to blunt the ongoing danger of the virus by asking people to stay home.
"We have 20,000 people hospitalized, over 2,000 people dying per week from COVID right now. And it is more dangerous than the flu and other respiratory infections," she said.
A new "pan-respiratory approach"
Agency officials had said last year they were working on plans to draw up a new "pan-respiratory approach" to its recommendations, combining guidance for COVID-19, influenza, and RSV, but those were not finished in time for this winter virus season.
"It's not something that ended up happening for this fall. Definitely still being considered for the future," Brendan Jackson, head of the CDC's COVID-19 response, told state and local health officials last November.
It is unclear how far the agency's draft changes are from being finalized. In the past, proposed revisions to the CDC's COVID-19 guidance have changed as the agency consulted stakeholders and did modeling and analysis of its impacts.
A person familiar with the discussions said the agency had begun outreach to some outside health experts and officials about updates to its respiratory virus guidance, with the goal of finalizing them before next winter.
This comes after states and other countries abroad have already moved to ease their own COVID-19 recommendations.
As the official public health emergency wound down last May, health authorities in Oregon announced they would replace their five-day isolation recommendation with a plea for people to stay home only until they had gone 24 hours without a fever, if their symptoms were mild and improving. California said it would make a similar recommendation earlier this year.
"This change acknowledged that isolation alone (i.e., in the absence of additional protective measures such as universal masking) was doing almost nothing to halt transmission at the community level," Afiq Hisham, an Oregon Health Authority spokesperson, said in an email.
Hisham said data they shared with the CDC and other state health departments showed the change did not lead to "disproportionate increases" in the toll inflicted by the virus across Oregon.
"It's also important to consider that isolation is a policy that is typically used when the public health goal is to contain an infection. That is not OHA's goal. Our goal is to help people in Oregon make informed decisions to protect themselves from severe infection," Hisham said.
Not a big change for many
While ending the five-day COVID-19 isolation policy could mark a significant departure from the CDC's previous guidance, the shift may amount to little more than catching up to reality for many Americans.
"When people don't have the luxury to stay home, when they don't have paid sick leave, it can be very hard to get folks to stay home because they tested positive for five days," said Marvia Jones, head of the Kansas City Health Department in Missouri.
Jones said she was skeptical shortening the isolation guidance would have much of an impact in her community.
Some workplaces are also already offering less flexibility to stay home after testing positive, she said, or stepping up demands for doctors to confirm that people were sick with COVID-19. Even during the height of the pandemic, getting a doctor's note was a tall order for residents without primary care providers or worried about facing big bills for a visit.
"Some doctor's offices, they're even saying, 'we don't want to do testing. Don't come in here. If you have symptoms, take the test at home,'" she said.
Hospitals are also not expected to see big changes imminently.
A separate sweeping update to the agency's recommendations for managing the spread of COVID-19 and other infections specifically in healthcare settings is already underway. An early draft drew fierce criticism from the National Nurses United union last year.
The CDC says its updates to those guidelines will be "accomplished in stages over a period of several years."
"The COVID-19 pandemic has forever changed the approach we take in healthcare settings to protect healthcare personnel, patients, and others from transmission of respiratory infections," the agency said in a blog post in January.
New variants could pose a risk
Dr. Janak Patel, director of the department of Infection Control & Healthcare Epidemiology at The University of Texas Medical Branch, says he understands the shift, but worries if future variants could disrupt this step toward a "new normal."
"We have to be very cautious that perhaps another variant that escapes our immunity completely may emerge and may require different precautions," he says. "Once we make policy in this forward manner, if we had to have a situation where we would need more caution, it will be very hard to go back to more prolonged isolation."
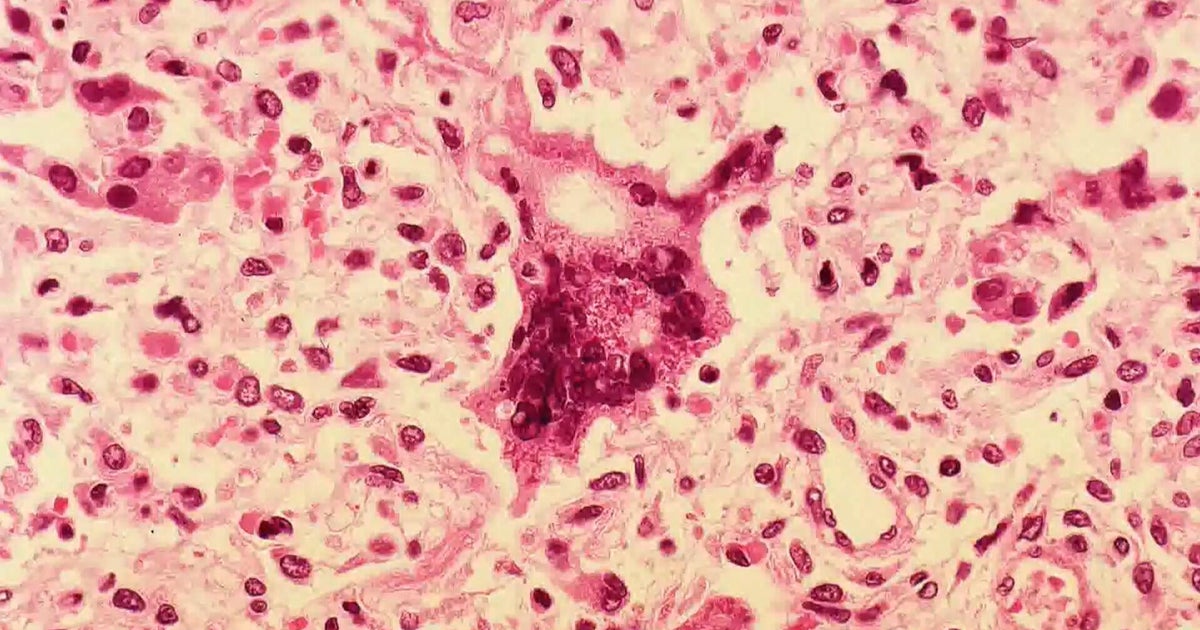
On Friday, the CDC said it had begun tracking a new highly mutated variant spotted in South Africa called BA.2.87.1. While strain does not yet appear to have gained a foothold outside of the country, other potentially worrying variants have been able to mutate to spread faster.
"Experience with BA.2.86 demonstrates that the ability of the virus to transmit can change quickly over time," the agency said, referring to the strain last year that later evolved into the now-dominant JN.1 variant.
Even with current variants, experts worry about what this may mean for people who are most vulnerable.
"Frankly, there has been no change in the science. Most people continue to be shedding virus for about nine days, with a range of six to 11 days," said Dr. Lara Jirmanus, a clinical instructor at Harvard Medical School and member of the health watchdog group called The People's CDC. "Younger patients will tend to be infectious for maybe one day less than that. Older patients or people with severe disease can shed the virus for a longer time."
Patel worries that if isolation begins to be viewed as unnecessary, vaccination will as well.
"Over time, immunity from both natural infection as well as vaccination subsides… so we need to continue to focus on prevention with vaccination in order to live life as normally as possible, including reducing the number of days to stay home — yes, that's a benefit — but we need to continue to keep our immunity up if we have to benefit from this relaxation of new guidelines."
Any shortened isolation recommendations will make vaccination as well as masking vital, adds Dr. Joëlla Adams, an epidemiologist in the Center for Applied Public Health research at nonprofit research institute RTI International.
"Vaccination will be an even more important strategy to prevent severe illness, particularly for individuals at higher risk of complications with COVID," she says. "It is not too late to get the updated COVID vaccine."