Unraveling a genetic clue to our "sixth sense"
Two young patients with a rare condition have helped scientists unlock a better understanding of our sense of touch and what researchers call our “sixth sense” – our physical awareness of our place in space. The work has identified a gene involved in both.
The girls, ages 8 and 18, were born with an array of health issues including dislocated hips, finger and foot deformities and curvature of the spine, called scoliosis. Both have had walking and balance problems since birth. They’ve also both had unusual experiences with their sense of touch. Yet, they can sense temperature and pain and have no muscle weakness.
They met scientists from the National Institutes of Health, where they underwent a series of tests including brain imaging, whole genome sequencing and exercises that evaluated movement. The findings are described in a study published today in the New England Journal of Medicine.
Certain test results offered deeper clues into their condition, said the study’s lead author, Alexander Chesler, an investigator at NIH’s National Center for Complementary and Integrative Health. He highlighted a simple exercise that evaluated the ability to sense the body’s place in space – called proprioception.
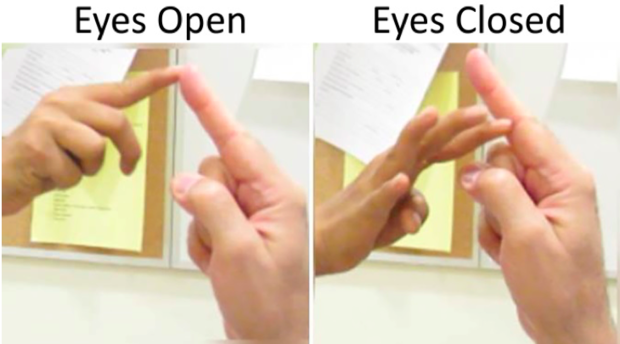
The scientists found that while both young patients could negotiate their way across a room or touch the palm of a study investigator with their hand with eyes opened, when they were blindfolded, they stumbled while walking. And during the palm test, their hands “danced” in space, unable to find the target.
Without looking, neither of the patients could guess the direction their hands or legs moved as well as control subjects who went through the same tests.
“In the older patient, when her eyes were open, when she was paying close visual attention, she could see where she was going. But when you asked her to close her eyes, she had no idea where her joints were in space. Her hand, she didn’t know if it was going up, down, or sideways,” co-lead author and pediatric neurologist Dr. Carsten Bönnemann told CBS News.
“We see loss of joint position sense in nerve disorders. But nerves get affected according to their length and so you may see this loss just in the feet or fingers, but it was very unusual that we saw it lost in all the joints of her body. Something had knocked it out specifically,” said Bönnemann, who is senior investigator and Chief of the Neuromuscular and Neurogenetic Disorders of Childhood Section at NIH’s National Institute of Neurological Disorders and Stroke.
“This is proprioception and it’s a very selective deficit,” said Chesler. In healthy people, it’s described as body awareness, “something you feel through your skin and bones,” he said, and it’s an essential quality most of us take for granted.
For example, proprioception helps us find our way in the dark to the bathroom at night. It allows musicians to play the piano without looking, and it guides Olympic gymnasts from bar to bar as they swing through a routine – it’s a “sixth sense” of sorts.
Several other tests provided more fodder about the nature of the condition. The patients couldn’t feel vibrations from a buzzing tuning fork as well as control subjects did, or the gentle stroke of a soft sable brush against the palm. But both patients could feel the brush when it was stroked up higher on their arms, on an area with hair.
“When we did that experiment – brushing the palm versus brushing the forearm – we did them in the fMRI scanner, looking for relative changes in brain activity. When you brush their palm, there’s no elicited brain activity we could measure, but we could see activity in the brain when we brushed their arm. But the activity in their brain was different from the control patients,” Chesler said.
The patients also described the brush feeling as “prickly,” he said. “Not like what you or I would say was soothing or comforting. Their vocabulary is just different. The way to describe them is different. It allows us to go back to my lab and guide our research back to basic science. My lab is interested in how the nervous system encodes touch and pain, how do we detect these things,” he explained.
Understanding “touch blindness”
Bönnemann and his group performed the exome sequencing, found the mutations, then contacted Chesler’s lab.
Chesler said mutations in “touch sensor” had been previously found in mice by another lab, and this helped them make the connection that mutations for “touch blindness” exist in humans. The gene involved is called PIEZO2. In the two patients, mutations in the gene appear to block the normal activity of proteins there.
PIEZO2 is what scientists call “a mechanosensitive protein,” he explained. It helps create signals when skin cells and neurons in the hand or feet touch different surfaces – a flat, smooth floor or a rough, sandy beach, for instance. In mice, PIEZO2 is found in the neurons that control touch and proprioception. But almost nothing is known about the role of PIEZO2 in humans.
In these two young patients, the scientists suspect the gene PIEZO2 may not be working correctly.
“‘Touch-blind’ people had not been identified before, and these are the first well-documented cases of someone with specific types of touch and proprioception blindness. It tells us what this particular sensor is critical for. But also seeing what the patient has left reveals to us all the things we don’t know. As a scientist, that’s even more important,” Chesler said.
Mayo Clinic neurologist Dr. Christopher Klein, who was not involved with the study, sees many patients with rare diseases. He told CBS News it is an important study.
“What this article is highlighting is that there’s a significant amount of sensory loss selective to a group of fibers that help us know where our bodies are in space. Things we take for granted,” said Klein.
“Papers like this are really important. They help us get at the mechanism – how is that mutation injuring the nerve or spinal cord? It highlights the importance of individualized medicine,” he said.
Bönnemann noted that the young women in the study have very healthy brains.
“The brain is completely normal. Both of these kids are really bright. The older one is in college,” he said.
It was striking how both were able to find ways to make up for the gaps in their perception, Bönnemann said – “how much their nervous systems compensate for their lack of touch and body awareness. It is surprising how functional someone can be without it.”
No sense lives alone, he noted, and their finding suggest that the nervous system may have other alternate pathways that researchers can explore when coming up with new therapies, but those therapies won’t be simple to develop.
“This is a huge gene. It’s way too big to be able to replace with gene therapy,” said Bönnemann.
Until specific therapies are available, patients can learn to focus on other coping tools, said Mayo Clinic’s Klein.
“Most of the kids I see back as adults, they learn to use their eyes. We want to make sure their eyes are good, that they visit the ophthalmologist.”
Making sure their home is well lit at night, eliminating fall risks such as throw rugs and uneven flooring, can help.
He said he talks with kids and adults who have proprioception and touch issues the way a driver’s education instructor teaches teens: to be aware that when they are nervous or in the dark, if they’re experiencing “bad road conditions” or someone is distracting them, that they need to stay focused.
“Using their good brains, they can largely prevent a lot of falls,” said Klein.
Chesler said the study has created more questions – but he’s looking forward to tackling them.
“Touch is one of our most critically important senses. I would argue touch is the most associated with intimacy. We know so little of it and we have a lot more to learn,” he said.