Why do COVID-19 PCR and antigen tests produce different results?
COVID-19 tests are in greater demand than ever, and new data about the Omicron variant can make picking and using different types of tests confusing. Molecular tests for COVID-19, like the "RT-PCR" technology used by many laboratories — known as PCR tests — are widely considered the "gold standard" for spotting the most infections caused by SARS-CoV-2.
By comparison, "antigen" or "lateral flow" tests, which can be done at home and return faster results, are less sensitive than PCR tests, but could be useful for identifying cases when people are likely to be contagious. One review last year estimated rapid antigen tests might only detect on average 75% of cases that PCR tests can spot, with antigen tests performing best in symptomatic people within the first week of their disease.
Some public health officials have advocated for wider adoption of antigen testing by Americans — if they can manage to find one of the rapid at-home tests — as an added layer of protection that might spot more cases before they spread.
But many factors can affect how likely a COVID-19 test is to accurately spot an infection. Here's the latest on how these two types of tests work and why they might sometimes offer different results:
A refresher: How PCR and antigen tests work
Most laboratories generate their COVID-19 test results through a molecular testing process called reverse polymerase chain reaction, or RT-PCR, that has been used for years to diagnose a variety of diseases.
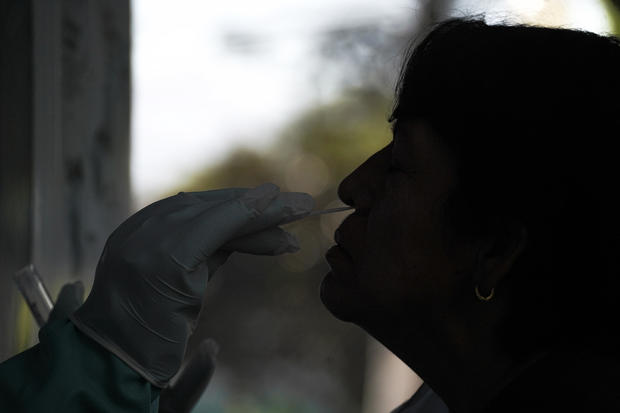
A patient gets tested with a nasal or throat swab, or in some cases provides a saliva sample. Then, using chemicals and specialized equipment, scientists mix the sample collected from the patient with the ingredients needed to create copies of the genetic material that makes up the virus. By repeating many cycles of this process, special sets of primer and probe chemicals can be targeted by test manufacturers to look for distinctive signs of SARS-CoV-2 — the virus that causes COVID-19.
"The PCR test, it's looking for that genetic material inside the virus and you don't have to have a huge viral load to pick up for it to be sensitive and specific, meaning it functions extremely well under a variety of circumstances to include the asymptomatic as well as the symptomatic," said Dr. Emily Volk, president of the College of American Pathologists.
"PCR tests are still by far the best test and those are the tests that most hospitals are using to identify COVID-19 patients," she said.
In addition to PCR tests offered at medical offices, pharmacies and drive-thru and pop-up testing sites, some test kits allow people to collect their own sample at home and then send it off to a lab for PCR testing. These are different than the rapid at-home antigen tests that return results on the spot.
The FDA has also authorized some test options from Detect, Lucira, and Cue Health that allow families, business owners or private facilities to collect samples and run a type of molecular testing similar to PCR themselves, but the equipment can be costly.
Antigen tests are a popular at-home alternative to those molecular tests, though they remain in short supply at many stores and online retailers. More than a dozen companies have been granted authorization to sell antigen tests over-the-counter, which can yield results at home in as little as 15 minutes.
These tests work by mixing samples from patient swabs with a buffer, a liquid that helps the virus travel across a strip coated with antibodies that bind to specific proteins — known as antigens — common to many variants of the virus. Similar to a positive over-the-counter pregnancy test, the strip appears as a colored line if it detects the antigen.
Different types of free or low-cost COVID tests are available at sites around the country. Find a location near you.
Starting this month, the White House says it also plans to offer a website to distribute free at-home tests online, and will require health insurers to reimburse for the purchase of at-home tests.
Are tests as good at detecting Omicron?
Only a small handful of the molecular testing kits used by laboratories have been found to fail to detect COVID-19 cases caused by Omicron, according to the Food and Drug Administration, because of mutations that evade the targets picked out by the developers of those tests.
On the other hand, a partial target failure seen with some PCR test brands, known as "S-Gene Drop Out," has actually been helpful for laboratories because it helps them quickly identify potential Omicron cases for genetic sequencing.
Since antigen tests generally target a part of the virus called the nucleocapsid, which saw fewer mutations in Omicron, test manufacturers and health authorities abroad say antigen tests should still work to detect many cases caused by the variant.
On December 28, the FDA said early studies by the National Institutes of Health turned up signs that antigen tests were able to detect Omicron but might have "reduced sensitivity" to spot cases of that variant compared to other strains.
The NIH's early research found that in test-tube studies, some over-the-counter antigen tests could only detect Omicron at higher concentrations than were needed to detect Delta. But they noted that this would not necessarily result in a significant drop in real-world performance — which is now being tracked by researchers.
"A change in sensitivity in the laboratory is not a guarantee that there's a change in sensitivity from a clinical point of view. I would not recommend that people suddenly abandon their antigen tests," said Bruce Tromberg, head of the NIH RADx effort that had run the studies.
Why different tests may yield different results
While PCR tests can be highly sensitive at detecting cases of the virus, health authorities caution that people can continue to trigger positive PCR test results for weeks or even months after they may feel they have recovered — "long beyond the period of expected infectiousness."
One CDC cohort study published in October found people were shedding fragments of the virus that could be spotted by PCR tests for an average of 30 days. However, scientists in several studies have generally been unable to culture live virus — a resource-intensive way that scientists can try to assess if someone is actually capable of spreading COVID-19 to others — from samples collected later than 9 days after symptoms begin.
This is part of why the CDC exempts people who have recovered from COVID-19 in the past 90 days from its international pre-flight testing requirement — they might still get a positive PCR test result even though they're no longer sick.
By contrast, while antigen tests may not be as sensitive as PCR tests in spotting every COVID-19 case, research with previous variants found using antigen tests two days in a row could reliably spot many cases of the virus when people were very infectious.
One study co-authored by CDC scientists, published in August, found repeated antigen testing in nursing home residents spotted all the positive cases that were verified by other lab tests.
"The appropriate tool in this pandemic to answer the question, 'Do I need to isolate? Am I infectious and a risk to my neighbors?' is using a rapid antigen test because it only stays positive as long as you are infectious," epidemiologist Dr. Michael Mina, the chief science officer at eMed, told "CBS Mornings."
The CDC also recently laid out guidance for using antigen tests to help decide whether to end isolation after you've tested positive for the virus but have no symptoms. A negative test is not required to end isolation, but the CDC called it the "best approach."
What you should do with results from an at-home test
After you first get sick, because of antigen testing's lower sensitivity as well as the small possibility for false positive results, health authorities have repeatedly urged Americans to seek out PCR tests to confirm whether they are infected with the virus.
Some local health departments are also urging residents to voluntarily report at-home test results to them. A spokesperson for Washington state's health department says they've received more than 1,310 positive test results since August through a hotline they set up, in addition to results reported in the state's smartphone app.
Unlike PCR tests, which are generally performed by laboratories that report summaries of their results to government agencies, public health experts and watchdogs have warned for months that growing use of at-home tests could hinder accurate tracking of COVID-19 cases in the U.S.
Meanwhile, test positivity rates have soared beyond recommended thresholds in every state, according to a tally by Johns Hopkins University — a sign that the reported test results are not capturing a significant share of the virus currently circulating in the community.
Testing for virus in the throat?
Anecdotal reports have emerged suggesting that swabbing the throat in addition to the nose — as some antigen tests in the United Kingdom require — might improve the odds of spotting an Omicron case. Some early studies also suggest that samples collected from saliva might be able to spot Omicron cases earlier.
The idea has picked up traction amid preliminary research suggesting Omicron might spread faster first in the upper respiratory tract instead of the lungs.
For Americans, trained health care providers can already collect and run tests on these types of "oropharyngeal" samples. But at least for now, over-the-counter COVID-19 tests have only been greenlighted by the FDA for use with nasal swabs.
"We generally do not believe that throat swabs are appropriate for self-collection. If performed incorrectly they can cause harm," the FDA's Toby Lowe told test developers in October.
Another way to improve the odds of successfully detecting the virus is to simply take another at-home home test 24 hours later.
Volk said the possibility that antigen tests might perform better in the throat deserved more investigation, but warned that not carefully following the directions on antigen tests can lead to mistakes that hinder a test's accuracy.
"Today I would say, still follow the instructions of the rapid test that you're using and collect it the way they tell you to collect it," said Volk.