Loss of smell or taste was once a telltale sign of COVID. Not anymore.
Once a hallmark sign of many COVID-19 cases — sometimes more reliable than even flu-like symptoms at sniffing out people infected by the virus early in the pandemic — was the sudden loss of smell and taste. But growing research suggests this symptom has become far less common, with only a small fraction of new patients reporting it last year.
The findings come from analysis of a sweeping dataset of medical records gathered by the National Institutes of Health for COVID-19 researchers from around the country.
"In the past, people were quite aware, if they had a cold and they lost their sense of smell, that they potentially had COVID. Whereas now, you really can't tell," Dr. Evan Reiter, medical director of VCU Health's Smell and Taste Disorders Center, told CBS News.
Reiter led the study, which was published in May in the journal Otolaryngology-Head and Neck Surgery, examining odds of patients with COVID-19 also reporting loss of smell and taste.
While the symptoms known as chemosensory loss occurred in an estimated 50% of cases early in the pandemic, the latest research suggests a prevalence of just 3% to 4% in more recent Omicron waves.
The study is among the latest to illustrate how the symptoms inflicted by the virus have changed, as new variants have emerged and immunity from infections and prior vaccinations offer defenses that early patients lacked.
Researchers from University College London reported in a study out last week that the proportion of cases reporting loss of taste or smell had significantly decreased after the Omicron strain emerged in 2021.
As more variants of concern emerged, "SARS-CoV-2 symptomatology gradually resembled that of other respiratory symptoms. The more contagious Omicron strains were significantly associated with an increase in cough and sneezing," that study's authors wrote in the journal Scientific Reports.
A path to new treatments?
Scientists have more clues now to unravel why many patients may have not recovered their taste or smell after infections earlier in the pandemic.
A team of researchers, led by Duke University's Dr. Bradley Goldstein and Harvard University's Dr. Sandeep Datta, reported last year that a ramped-up immune response seemed to be still targeting nerve cells in the nose long after the virus had already dissipated.
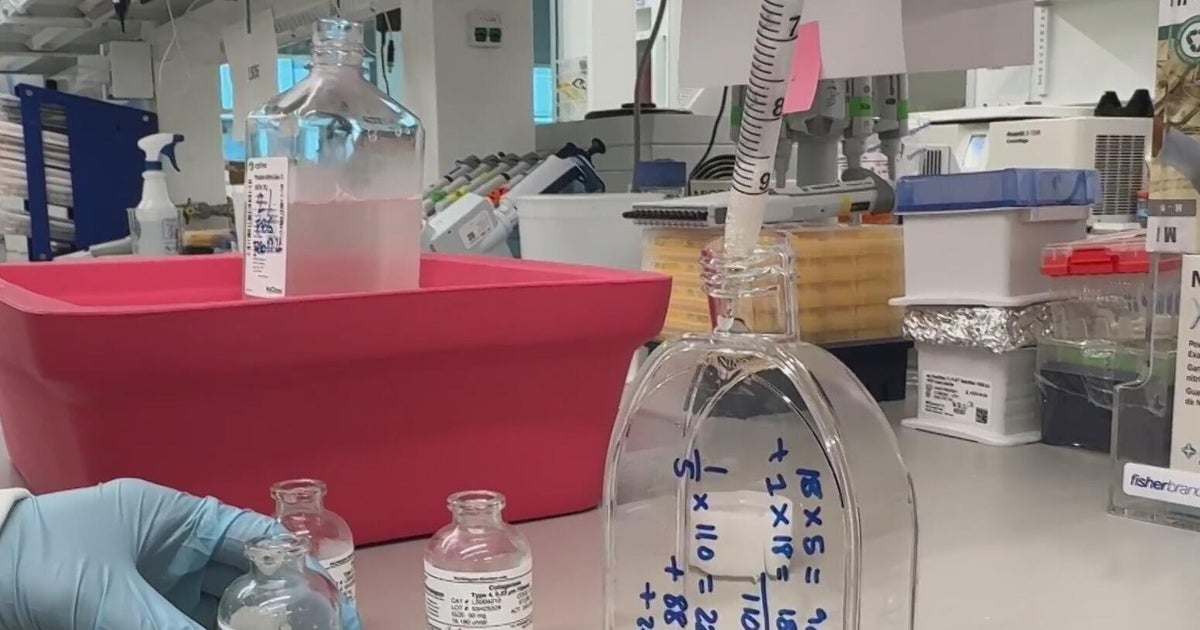
Volunteers allowed the doctors to scoop out a small sample of tissue from high up in their nose, which was then rushed back to their lab to be cleaned and filtered.
Those were fed into instruments that let them analyze the samples down to a single cell. These were compared against data from samples of other patients without this kind of smell loss, revealing signs of ongoing inflammation driven by the immune system's T cells. That amounted to the first living confirmation of a leading theory for long COVID smell loss, which had been based mostly from autopsies or experiments on animals.
"Accompanied by just overall fewer intact olfactory neurons or nerve cells in those long COVID smell loss biopsies, that combination suggests likely those immune cells are continuing to drive some level of ongoing damage or preventing repair," Goldstein, associate professor at Duke's Department of Head and Neck Surgery and Communication Sciences, told CBS News.
Goldstein said their findings echoed those seen driving some other persistent symptoms in long COVID sufferers, recalling meetings with other researchers convened by the NIH's RECOVER program.
"Whether it's the kidney, or the heart, or the brain, I think there's a common theme emerging that a lot of it seems like it's immune system mediated, and that was one of the big findings in our paper," said Goldstein.
This could pave the way to new treatments that might be able to make room for the body to rebuild its nerve cells for smell by directly curbing the immune response.
"I think this is where the olfactory loss field needs to go, more broadly, in the direction of what areas could be drug targets and may promote nerve cell regeneration or recovery," he said.
The NIH recently announced it had begun enrolling volunteers in trials of treatments for some long COVID symptoms, though none have specifically been announced for smell loss.
"Patients experience many symptoms," the agency said in a statement, adding, "the interventions currently tested or in process of being tested may sort effects on many of these symptoms, including loss of smell/taste."
Smell training and nose injections
For now, doctors only have a handful of options to try and treat patients still struggling with the loss of their sense of smell.
Beyond impacting one's quality of life, like distorting once-palatable foods into off-putting flavors, Reiter said patients struggling with this long COVID issue face a range of new challenges.
"Your nose serves as a little bit of an early warning system with smoke and fire, and you have a harder time detecting things like gas leaks, and even things like detecting whether or not your food is spoiled," said Reiter.
A common starting point for treatment is olfactory training, which works by repeatedly exposing the nose's damaged smell nerves to distinct categories of pleasant smells.
One drug treatment that has been tried is steroids, though Reiter said evidence of it working remains scarce.
Reiter said an approach that has shown some promise in pilot studies is using concentrated formulations of platelets drawn from the patient's own blood, which might be able to regrow tissue after being injected or soaked into the nose.
However, treatments can carry risks, and Reiter said many patients eventually recover their sense of smell on their own after little intervention by doctors. An earlier survey by Reiter's group found only 7.5% of patients continued to have no improvement in their sense of smell years later.
"A lot of the time, it really just is time. Nerves can recover," said Reiter.