What we know — and don't know — about immunity to the coronavirus
Scientists still have a lot to learn about immunity to the coronavirus. The World Health Organization has said there currently isn't evidence to prove people can't get reinfected with the virus — and even if they do have some protection after recovering from the virus, it's unknown how long that may last. Labs are working on developing a vaccine but it will take time.
Dr. Bob Lahita, a professor of medicine at New York Medical College and chairman of medicine at St. Joseph University Medical Center in New Jersey, explained on CBSN Friday what doctors know and don't know about immunity to COVID-19.
How does immunity work?
Lahita described two types of immune responses when the body is infected with a virus: the innate and the adaptive.
The innate response is "not specific" to the virus, Lahita said. "It's sort of like the body's SWAT team and that attacks whatever the invader is, in this case COVID-19 virus," he said.
Then, "about three to five days after the virus makes its appearance, it has on its surface proteins which distinguish it from other coronaviruses and other viruses like influenza. These proteins set up an adaptive immune response, which means your cells in your body make antibodies to the virus and this antibody response should be specific and very sensitive," Lahita said.
"The antibody to the virus is called a neutralizing antibody, which means that it takes the virus and attacks it and neutralizes it," he said.
Can we become immune to COVID-19?
While there are hopes that once someone has COVID-19 they can't get it again, Lahita said doctors don't know for sure if that is the case. Having antibodies to the coronavirus may not mean we are immune to it, he said.
"All of our normal immune systems make antibodies to this virus, and we would presume that we can neutralize the virus once it comes into our bodies, but we're not so sure that we cannot be reinfected later," he said.
Lahita used the flu virus as an example.
"We try to have neutralizing antibodies to viruses like influenza, but again, we can get that again," he said. "So our big concern and the WHO, the World Health Organization's, concern is, can we get this viral infection again? And the answer is we simply don't know."
Lahita also noted that there are many types of coronaviruses, so even if someone has antibodies against a different coronavirus it may not protect against COVID-19. Antibodies have to be specific to the virus, he explained.
There are concerns that there could be a resurgence of the coronavirus in the fall, the same way the common cold and the flu come and go, he said.
Will we have to get annual coronavirus vaccines, like the flu shot?
Flu shots have to be given every year because the influenza virus mutates.
"Every year, there's a little bit different kind of a virus that can infect us," Lahita said, so the flu vaccine needs to change too. "We know about influenza A and we know about influenza B, but we need to have a boost. Our adaptive immune system has to be shown the virus to provide us with a boost of neutralizing antibody."
Lahita said he expects the same thing will happen for COVID-19.
"We're probably going to package the two vaccines together so that when you get your flu shot in the fall and into the winter, you'll also get your COVID-19 flu shot once the vaccine's available," he predicted.
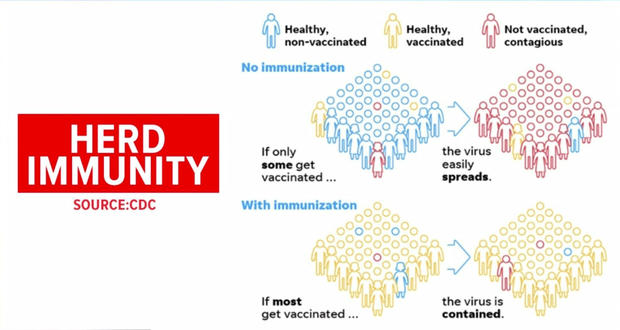
What is herd immunity?
Herd immunity is "what we want to see," Lahita said. "That means over 70% of the population has been infected and has antibodies." Once a large enough proportion of people are immune to an infectious disease, it can't spread easily within the community.
Lahita said we have seen herd immunity work with other diseases, such as polio.
"That's the perfect example of what we want to see going forward, which will protect all of us, put us all back to work and everything will be back to normal again," he said.