Building bridges to combat COVID-19 in communities of color
As protests against police brutality began in late May, Kechia Matthews lay in a hospital bed battling COVID-19: "I really could not breathe at all. Like, I just felt no air, no nothing. It was scary. It was terrifying. It happened fast. I didn't know where it came [from], like, it just hit."
She was treated by a team of doctors at Johns Hopkins University, including Dr. Panagis Galiatsatos, who said, "I couldn't forget how she looked, the fear in her eyes realizing she could die."
Matthews, a Baltimore native, was just about to graduate with a degree in criminal justice and forensic science from Coppin State University. But it wasn't clear if she'd survive. "I've never been as scared in my life," she told correspondent Allison Aubrey of National Public Radio. "I didn't think I was coming home. It was hard."
Young adults are much less likely to die from COVID-19. Dr. Galiatsatos said, "Kechia was telling us her preexisting conditions. As soon as she said diabetes, I mean, my heart sank, right? I wasn't just dealing with now a 27-year-old; I was dealing someone with one of the variables that we know is gonna create a likelihood of worse symptoms."
According to the Centers for Disease Control and Prevention, people with chronic diseases (such as obesity, heart disease and type-2 diabetes) are a staggering 12 times more likely to die from the coronavirus.
And Black Americans have a higher prevalence of these conditions.
Matthews was in the hospital for three weeks, and on a ventilator six days. When she was finally released, she emerged with a new sense of urgency: "Taking my health seriously; I need to," she said. "I don't ever wanna be put in a situation like that again."
But her determination is just one piece of the COVID puzzle. The lifestyle changes needed to tackle chronic disease are often difficult to make in economically-challenged areas.
Dr. Galiatsatos said, "One of the reasons why we see disparities ravage in the minority populations is because those kind of lifestyle requests are really hard to do in neighborhoods that are plagued by homicide, neighborhoods that are plagued by food deserts. And the challenge there is, resources to give them the opportunities to overcome that, were at a pace that, in my opinion, is unethical."
"People are now hungry and they are hurting," said Hassan Amin, who is imam at Masjid Ul-Haqq, a mosque in West Baltimore. "They were hungry and hurting before the virus. Now they're really doing so, because a lot of times the people we serve, these are the ones that are the last hired, first fired."
Dr. Galiatsatos has teamed up with faith leaders, including Imam Amin, to address these obstacles. At a community event at the mosque where fresh produce and grocery gift cards were being handed out, Dr. Galiatsatos answered questions about COVID-19. His goal: to build relationships. "Medicine is a public trust. We can't just know the science, right? We have to know the patient, and we have to know the community."
"So, by bringing him here, you're building bridges?" asked Aubrey.
"Oh, yeah," Imam Amin replied. "It was building bridges, filling in gaps. 'Cause right now, the people don't trust hospitals and doctors."
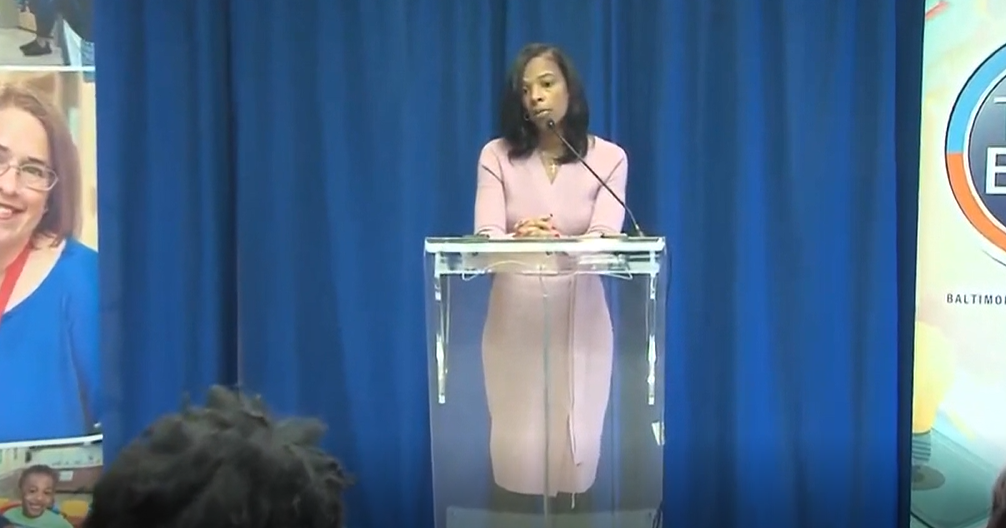
The hope is that partnerships between between doctors and community leaders (like Imam Amin) can help build trust. The strategy of working with so-called "trusted messengers" is backed by physician Sherita Golden, who is the chief diversity officer at Johns Hopkins Medicine.
"The reasons those trusted messengers are so important is that there are many of these vulnerable communities that are distrustful of the healthcare system, so this is because of prior historical experiences," she said.
From the infamous Tuskeegee syphilis experiment in the 1940s, when treatment was deliberately withheld from Black men, to Dr. James Marion Sims in the 1800s, who performed surgical experiments on enslaved Black women with no anesthesia, the history of racist mistreatment of Black Americans by the medical establishment is well-documented.
And what still persists today is the misperception that Black people are somehow different from other groups of people. Dr Golden said, "There's been sort of this questioning that, 'Are African Americans more genetically or biologically vulnerable to contracting COVID-19?' And there is no evidence of that. There is nothing genetic or biological about working in a service sector where you have to be essential, and you're just gonna get exposed because you happen to be there. So, there is no evidence that genetics is playing into this at all."
But another factor that likely is playing into this: Stress.
"Stress can make people more prone to infection," Dr. Golden said. "So what happens is that, it alters your body's immune response so that you may be less likely to be able to fight infection as well.
"Structural racism, that induces a form of chronic stress, thinking about, 'Where is my next meal going to come from? I've gotta work three shifts tonight. And then, I have to worry about my child getting pulled over by the police.' Like, those chronic stressors, even though you may not feel you are acutely stressed, they are still impacting your hormonal system."
Looking back, COVID-19 survivor Kechia Matthews says she was under tremendous stress when she got the virus: "Working a full-time job. Going to school. Seven classes at one time. Two hours of studying. Three hours of sleep."
And all of that takes its toll. Imam Amin points out Black people in Baltimore – and around the country – are more likely to have the types of jobs that you cannot do from home: "That means that they are exposed to all kinds of people all day long, coughing and sniffling, whatever, and then they end up maybe catching something, and they end up taking it home to their families."
It's one more reason why Blacks and Latinos are about three times as likely to get COVID-19
But Matthews said she's now full of hope. When she emerged from the hospital to see "Black Lives Matter" painted on streets, and White people joining Black people to protest injustice, she saw it as a symbol of progress.
Her goal is to become an FBI Special Agent: "That's my next career goal. And that also goes along with me and my health goals. You know, you have to be healthy, fit, in shape. So, another thing that's motivating me."
And Dr. Golden said that Matthews deserves a country that rewards that determination: "This is an important time for us as a country to really think about what are the things we value, what do we want to focus on, and how can we use our power of legislation to really address the issues of making our communities healthier, making our communities safer."
Aubrey asked Matthews, "What do you think your role is in pushing for change in your own community?"
"I want my people safe," she replied. "I want them to have someone they can trust. I want to have someone they can look up to."
"You seem hopeful."
"I am hopeful and determined," Matthews replied. "I'm gonna always be hopeful."
For more info:
- Medicine for the Greater Good, Baltimore
- Dr. Panagis Galiatsatos, Johns Hopkins Medicine
- Dr. Sherita Hill Golden, Johns Hopkins Medicine
- Masjid Ul-Haqq Mosque, West Baltimore, Md. (Baltimore Heritage)
- Muslim Social Services Agency, Baltimore
- Islamic Relief Worldwide, Birmingham, England
Story produced by Amol Mhatre. Editor: Ed Givnish.