After cancer-prevention surgeries, women learn BRCA gene test may have been wrong
Seven women in one family had major surgery after a widely used genetic test, taken by hundreds of thousands of people, showed a high cancer risk. But years later, the family has learned the results of that BRCA test might have been wrong.
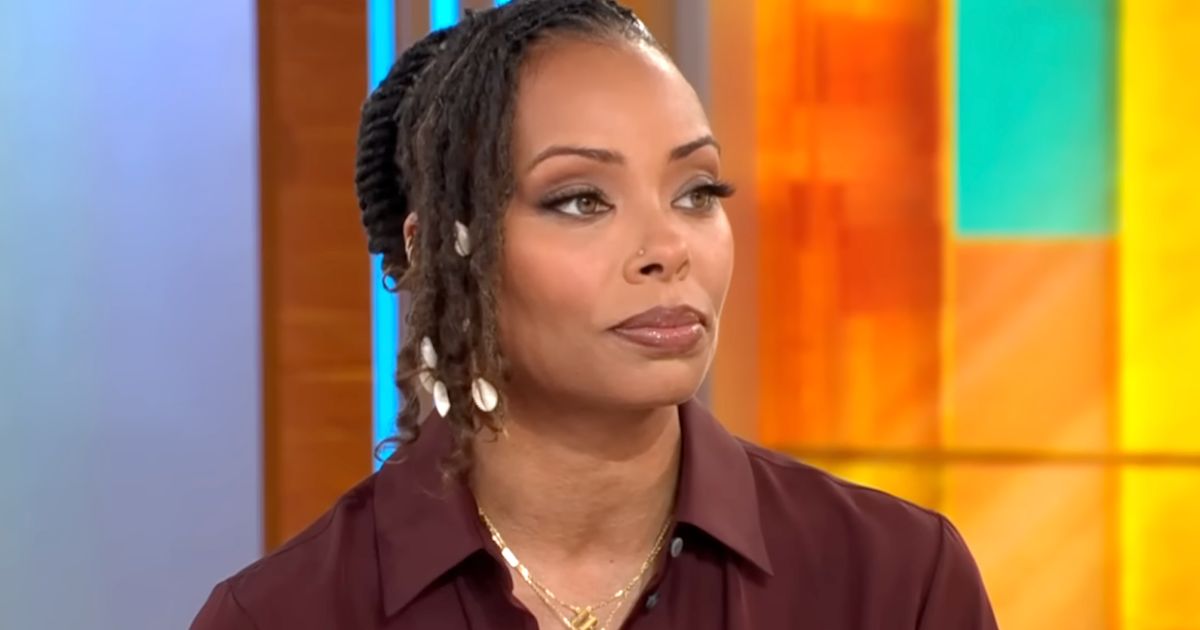
Katy Mathes, a teacher, was in her early 30s and married with a young son, when she decided to take a genetic test to check her risk for cancer. Shortly after, she learned she had a mutation on a BRCA gene, which significantly raises a person's risk of developing breast or ovarian cancer.
"It was very alarming," she said. After struggling over what to do, she underwent surgery to remove her ovaries and fallopian tubes and had a double mastectomy.
The recovery process was long, Mathes told CBS News correspondent Jamie Yuccas.
"It was nine months before I was cleared to pick up my child," she said. "I wasn't able to do bathtime with him. I wasn't able to make dinner for him. ... I wasn't able to pick him up or hug him for a very long time."
Her mother, sister, cousins, and aunts all got tested, too. Eleven had the mutation. Seven had surgery.
But four years later, Myriad Genetics, which did the test, told her and her family their risk assessment had changed.
"I went from 'very high risk,' 84%, to nothing," Mathes said. "It really felt like I was doing something for my family. I needed to do these surgeries to save them. And then, just the reality that I didn't need to do any of that was really heavy."
Myriad said such reclassifications are "extremely rare" and "as the science evolves, we scrutinize any new information and reclassifications are made only after very careful consideration."
"Hereditary cancer risk assessment is an important option for millions of people with a family or personal history of cancer and who meet medical guidelines for genetic testing. Myriad has more than 20 years of experience providing accurate genetic test results. Our test results interpretations are based on medical guidelines and the best available science at the time," Ron Rogers, executive vice president of corporate communications at Myriad, said in a statement.
"As the science evolves, we scrutinize any new information and reclassifications are made only after very careful consideration. The vast majority of reclassifications in this ongoing program are from an uncertain interpretation to one that is more definitive, which is highly desirable to patients. Reclassifications from pathogenic to uncertain are extremely rare and patients must still be managed according to family history. We strongly encourage anyone who has questions about genetic testing to speak with a healthcare provider."
CBS News medical contributor Dr. David Agus, a cancer specialist, said as more people take genetic tests, the results are improving.
"This is a changing, dynamic field where we're learning something every day," he said. "Right now, we've tested hundreds of thousands of people with this BRCA test. Every person that's tested, and we then follow the outcome, the database gets stronger. We have more information."
Though reclassifications are uncommon, Mathes said for her, the impact is ever-lasting.
"I removed body parts, and I can't have children anymore because of this," she said. "I just don't feel like myself, and the weight of that is a really big burden and what do I do each day? I have to get up and keep going. I'm a mom and a wife and a teacher ... so you just keep going."
Mathes also is worried insurance won't cover her required follow-up surgeries since she no longer has the cancer classification.
Agus said at-risk patients should get this genetic test. He recommends going to a National Cancer Institute-designated center where counselors can answer your questions.