A mom's sudden pain was a deadly heart condition. An ultrasound on an iPhone helped save her life.
Sara Adair knows the symptoms of aortic dissections. The hospital analyst's father and sister each experienced the dangerous cardiac condition, when the inner lining of the body's main artery tears and causes the aorta to come apart.
Aortic dissections can be deadly, and are hard to diagnose. Both Adair's father and sister survived, but after her sister's aortic dissection at the age of 49, Adair was determined to learn why it had happened. She, her father and her sister were diagnosed with Loeys-Dietz syndrome, a rare genetic disorder that affects the body's connective tissues.
Adair, a mother of two, learned the symptoms, saw a cardiologist and had regular scans of her aorta. There were no warning signs. On July 22, 2024, she spent the afternoon attending sports tournaments and a pool party with her kids. It was just another day in a "super busy weekend," she told CBS News, and she felt "completely normal." When they finally got home at 9 p.m., she sat down to unwind.
"All of a sudden my chest started to hurt. It felt fine all day, completely normal, then just all of a sudden this crushing, horrible, chest pain I'd never felt before," Adair said. "It was long enough for me to think 'Oh, is this really what I think it is?'"
Sudden chest or back pain that moves into the neck is a key symptom of aortic dissection. It was exactly what had happened to Adair's sister. It was a feeling she had been dreading.
"The pain moved up to to my neck, and then I was like, 'Okay, this is it. This is serious,'" she said. "I got up to tell my husband to call 911, but I made it into the living room where he was and just collapsed on the floor."
What is Loeys-Dietz syndrome?
Loeys-Dietz syndrome is a rare genetic condition that affects the body's connective tissues. Aortic aneurysms and dissections are a common risk for a person diagnosed with the disorder, said Dr. Hiroo Takayama, the chief of adult cardiac surgery at NewYork-Presbyterian/Columbia University Irving Medical Center.
Managing the condition includes regular cardiology appointments and scans of the heart and aorta. Some patients may be prescribed heart medication, Takayama said, and patients can also receive a surgical treatment called aortic root replacement to prevent tears in the aorta.
Almost all Loeys-Dietz patients will need surgery on their aorta: It's just a question of if it will be a scheduled preventative procedure or an emergency one, Takayama said.
Adair had been having regular check-ups, but the tests hadn't showed anything worrisome.
"I'd gotten all the imaging that I was supposed to, but it just wasn't detectable until it burst," Adair told CBS News.
Making a rapid diagnosis when "time is also ticking"
Even though Adair knew what was happening to her, she struggled to communicate it to first responders. Her husband insisted that she be taken to the emergency room at Robert Wood Johnson University Hospital, where she worked. Paramedics conducted a diagnostic test that indicated she was having a "huge heart attack," according to Dr. Partho P. Sengupta, the hospital chief of cardiology who oversaw Adair's care team.
Despite similar symptoms, the treatment for a heart attack is very different than what a person having an aortic dissection will need, and that's part of what makes aortic dissections so deadly, Sengupta explained.
"Over 50% of people (with aortic dissections) never make it to the hospital. Of those who make it to the hospital, their time is also ticking, because with every one-hour you delay getting the right surgery, you have a 1 to 2% increase in mortality," Sengupta said.
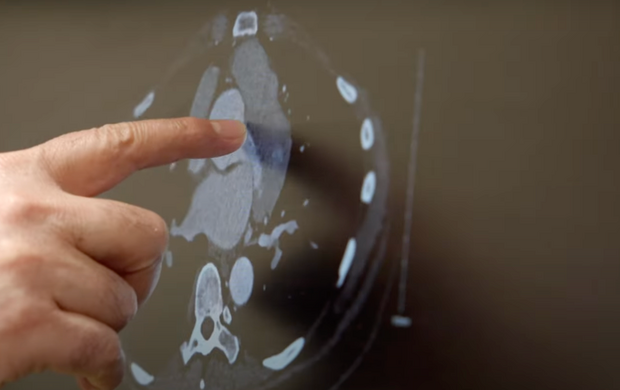
In the emergency room, a cardiology fellow was able to make the correct diagnosis. Dr. Shawn Chawla, who trained under Sengupta, used a point-of-care ultrasound to examine Adair. The device is a probe that plugs into an iPhone, turning the device into a portable ultrasound system. The scan showed the large tear in Adair's aorta, Sengupta said. Adair was sent for a CT scan to confirm the diagnosis, then underwent open-heart surgery performed by cardiac surgeon Dr. Hirohisa Ikegami.
"I know it was the ultrasound that I had in the emergency room that saved me," Adair said. "If I had been treated for a heart attack and brought, say, to the cardiac cath lab, or if I didn't go to the CT scan and get the diagnostic tests that I needed, I could have bled out."
Recovering after open-heart surgery
Adair had collapsed on a Sunday night, and she didn't wake up until Tuesday. She said she barely remembered anything that happened after she fell down.
The operation hadn't been without complications. She had had a stroke during surgery, which left her with some weakness in her left arm and slightly blurry vision. Fluid collected around her lungs and heart, creating breathing difficulties. She spent several days in the ICU.
Even after being released from the hospital, all Adair could think about was the night she collapsed and the terror she felt "knowing exactly what was happening, feeling it going up my neck, and knowing I had a really, really limited amount of time to get the right treatment."
She has spent months in cardiac rehabilitation and has several blood clots that still need to resolve. Despite the setbacks, she considers herself lucky.
"I think the worst already happened," she said.
The only thing she fears now is what genetic testing for her children and her nieces will show. The kids have appointments scheduled to be tested for Loeys-Dietz syndrome. If necessary, they will start seeing a cardiologist who can monitor their health.