Ambulance rides can be costly — and consumers aren't protected from surprise bills
Americans are protected from most surprise medical bills by the No Surprises Act that took effect last year. But there's one key item the legislation left out: ambulance rides.
A recent report found more than half of ambulance rides by insured patients result in a surprise bill. Those rides cost patients roughly $130 million a year, according to the U.S. Public Interest Research Group, or PIRG.
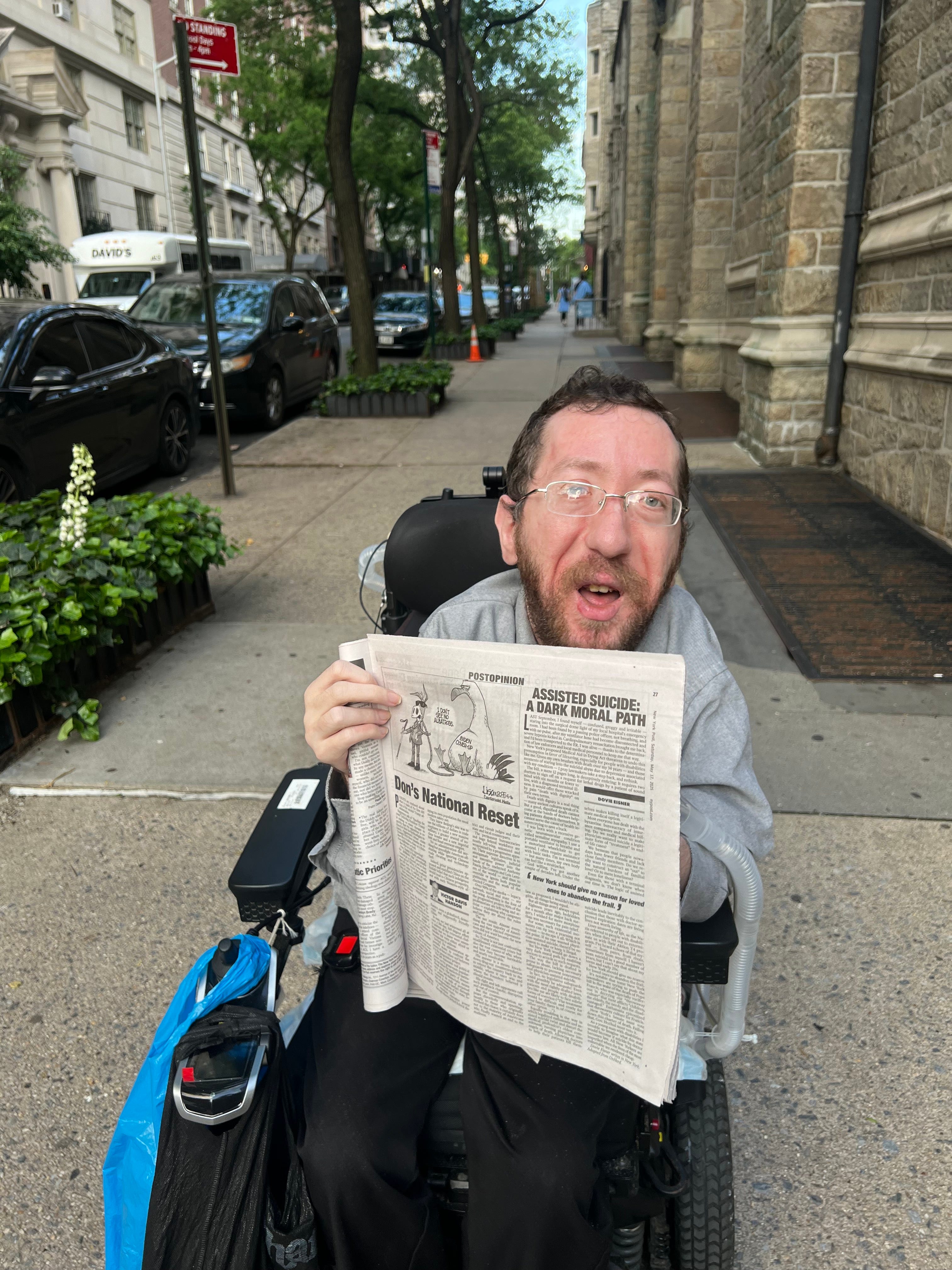
David Feng and Christy Shum are currently fighting their bill, which totals more than $7,000. The bill is for an ambulance ride their 1-year-old son, Theo, took from home as a newborn, a week after he was born prematurely.
"He was breathing, but very heavily," Feng said. "So he wasn't getting all the oxygen he needed."
Doctors told the couple the baby would need to be transferred by ambulance to a children's hospital with a special team and life support. At no point during that process did the cost of the ride cross their mind.
Yet a few weeks later, with Theo still hospitalized with what specialists determined were two holes in his heart, the couple got a bill for the ambulance transfer. It totaled over $7,000.
Christy's insurance company, UnitedHealthcare, paid nearly $1,000 of that, leaving them owing the rest – more than $6,000, because UnitedHealthcare said the service was an "out-of-network provider or facility."
"It's totally shocking when you see the bill and to me, it's really unfair," Feng said.
Many surprise medical bills like the one they received were eliminated by the No Surprises Act, legislation passed by Congress in 2020 that protects consumers against most surprise bills for emergency services, including life-saving helicopter flights.
But what it didn't get rid of were surprise bills from regular ground ambulances.
Patricia Kelmar with PIRG said Congress "dodged" the issue, and "decided to acknowledge the problem by creating a federal committee to look at the problem more deeply." Kelmar is on that committee.
"There are fixed costs when it comes to ambulance treatment," she said. "We should set a price that is tied to costs, and that will help make our insurance companies pay those costs, at a true price, and will protect people from these really high out-of-network bills."
But there's no firm timeline for developing a new system, leaving some families struggling.
Shum appealed their $6,000 ambulance bill, but got a letter from UnitedHealthcare saying: "Payment for this service is denied." The insurance company also took back the $1,000 it did pay – saying Feng's insurance company, Blue Cross Blue Shield of California, should have paid all the expenses for the baby's first month.
Over a year later, the ambulance bill – over $7,000 in total – remains unpaid despite hours spent on the phone with both companies, trying to get answers.
"It's frustrating," Shum said. "The fact that it's taking so much of our time and it's still not resolved and we still don't know anything."
The company that provided the ambulance told CBS News the bill had been submitted several times but had gotten "stuck" in the system. It also said specialized critical care transport is expensive to operate around the clock, and it relies on insurance companies to reimburse timely and at a fair rate.
Blue Cross Blue Shield of California told CBS News it couldn't answer questions about issues with the couple's bill due to federal privacy laws.
The family says Blue Cross Blue Shield called and promised it is working to resolve the issue, but the family says there's been no resolution yet.
UnitedHealthcare, Shum's insurer, said primary coverage for Theo was under his father's insurer, not UnitedHealthcare, but they have now "contacted both the ambulance company and (Blue Cross Blue Shield of California) to help get this bill resolved."
Still, Feng and Shum say the stress from the bills couldn't put a damper on a magical moment — the day Theo finally came home from the hospital after two and a half months. He is now healthy.
We'd like to know what you paid for medical procedures. You can email us at healthcosts@cbsnews.com.