South Florida Arrests Made In Connection To Multimillion-Dollar Healthcare Scam
MIAMI (CBSMiami) - Several arrests have been made in South Florida in connection to a multimillion-dollar healthcare scam.
In the first-ever nationwide COVID-19 fraud takedown, investigators say thieves attempted to capitalize off of the pandemic by using the personal information of patients and their DNA to submit faulty Medicare claims.
The Office of the Inspector General says, collectively, these scams resulted in more than $75 million in losses.
They say the accused thieves offered COVID tests to Medicare beneficiaries at places like senior living facilities, some drive-thru testing sites, and doctors' offices, but used their personal information and saliva or blood samples to submit faulty claims to Medicare for other unrelated tests.
Wednesday, The Department of Justice announced charges against 15 people across the country.
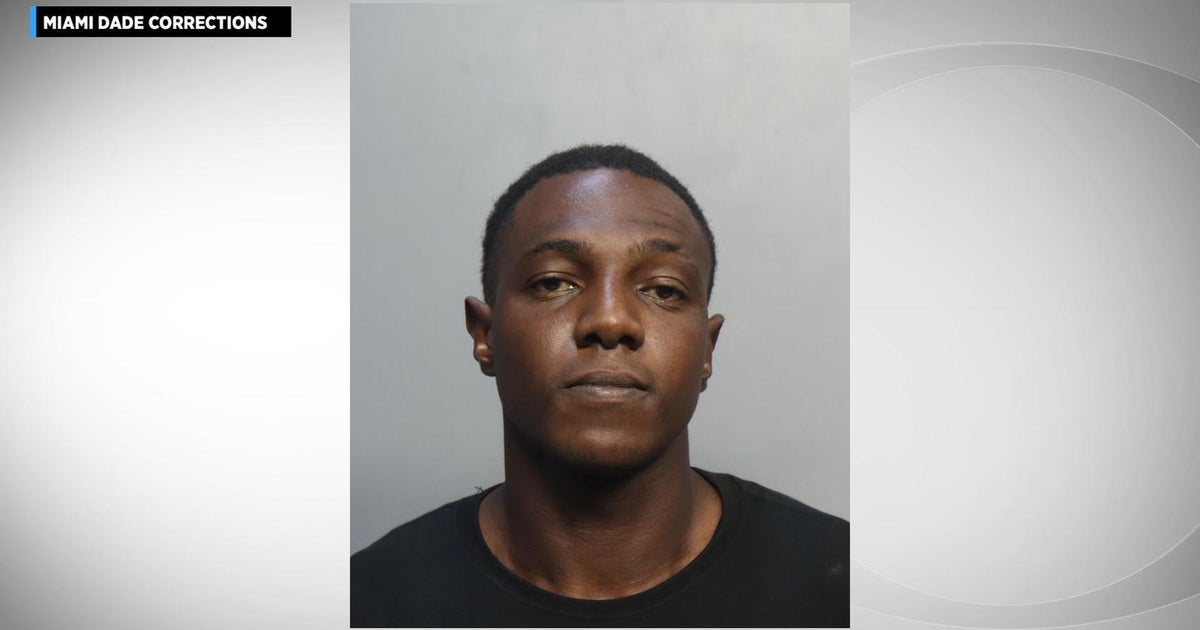
In South Florida, arrests were made for scams coming out of Boca Raton and Palm Beach County.
Juan Nava Ruiz and Eric Frank of Coral Springs, as well as Christopher Licata of Boca Raton, were charged for an alleged $9.3 million health care fraud, wire fraud, kickback, and money laundering scheme.
According to the Office of the Inspector General, Licata, an owner of Boca Toxicology, LLC, allegedly offered and paid kickbacks to patient brokers, including Ruiz and Frank, in exchange for referring Medicare beneficiaries to Boca Toxicology for various forms of genetic testing that they did not need.
In addition, Licata is accused of falsifying applications for COVID-19 relief funding, including applications and documentation for a $50,250 Paycheck Protection Program loan and a $150,000 Economic Injury Disaster Loan.
Leonel Palatnik and Michael Stein of Palm Beach County face charges connected to an alleged $75 million conspiracy to defraud the United States and to pay and receive health care kickbacks. Palatnik is owner of Panda Conservation Group, LLC, a Texas company that owned and operated testing laboratories.
Investigators say the two exploited the CARES Act by offering telehealth providers access to Medicare beneficiaries and billed them for consultations. In exchange, these providers agreed to refer beneficiaries to Panda's laboratories for expensive and unnecessary cancer and cardiovascular genetic testing.
Assistant Inspector General for Investigations Chris Schrank says the reason investigators caught on is due to the fact the Department of Health and Human services hotlines were receiving complaints that they were not getting their COVID test results back in a timely manner, if at all, which prompted the large-scale investigation.
Other suspects were charged in California, New York, New Jersey, Louisiana, Texas, and Arkansas.