How many Americans still haven't caught COVID-19? CDC publishes final 2022 estimates
Nearly 1 in 4 U.S. adults and older teens had still not caught COVID-19 by the end of last year, according to new estimates from the Centers for Disease Control and Prevention, while 77.5% had antibodies from at least one prior infection. The figures are based on the final batch of results from the agency's nationwide studies of antibodies in Americans ages 16 and up.
Federal officials often cited estimates from these studies in moving to simplify vaccine recommendations and loosen COVID-19 restrictions, as the Biden administration wound down the public health emergency earlier this year.
Virtually every American ages 16 and older — 96.7% — had antibodies either from getting vaccinated, surviving the virus or some combination of the two by December, the CDC now estimates. The study found 77.5% had at least some of their immunity from a prior infection.
Of all age groups, seniors have the smallest share of Americans with at least one prior infection, at 56.5% of people ages 65 and over. Young adults and teens had the largest proportion of people with a prior infection, at 87.1% of people ages 16 to 29.
Among the 47 states with data in the CDC dashboard, Vermont has the lowest prevalence of past infections, with 64.4% of Vermonters having antibodies from a prior infection. Iowa had the largest share of residents with a prior infection, at 90.6%.
Rates were similar among men and women. Black and White people also have similar prior infection rates, between 75% and 80%.
Among other racial and ethnic groups, Asian Americans had the smallest proportion of people with antibodies from a prior infection, at 66.1%, whileHispanic people had the highest, at 80.6%.
CDC estimates for children have already been published through the end of last year, using other data from commercial testing laboratories. According to those figures, a little more than 9 in 10 Americans under 18 had survived COVID-19 at least once through December 2022.
"Very difficult to measure"
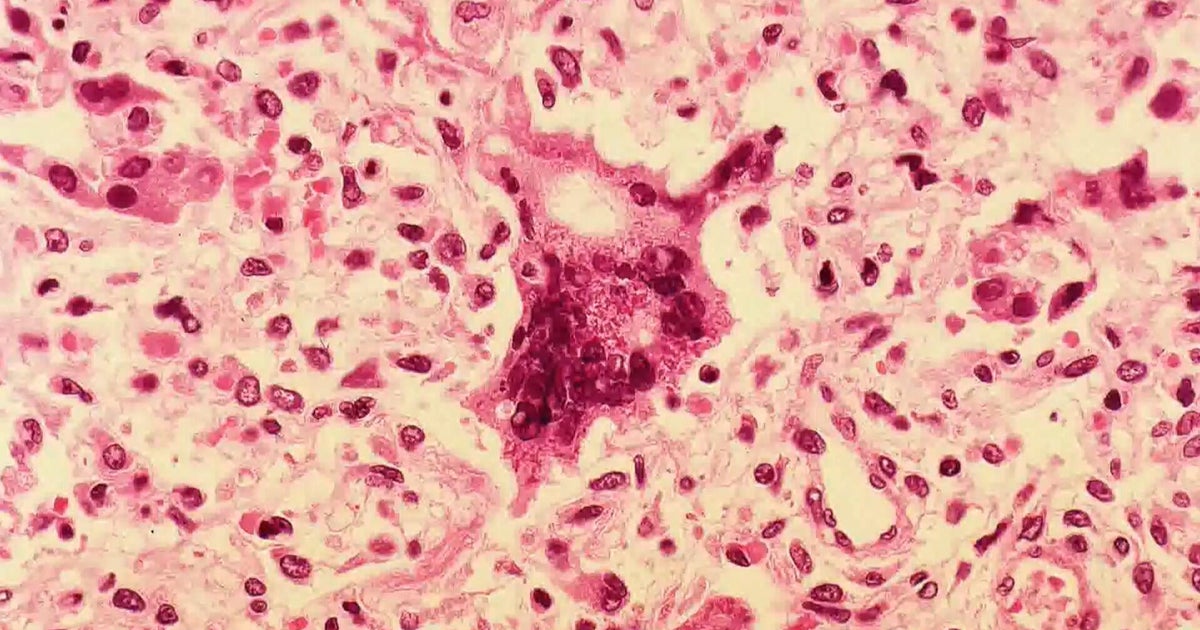
The federal figures on seroprevalence — meaning test results showing evidence of antibodies in the blood — had helped reveal how much the virus has spread undetected or underreported.
Just 54.9% of all adults currently think they have ever had COVID-19, according to Census Bureau survey results published by the CDC through mid-June.
Having antibodies from a prior infection does not mean people are protected against catching COVID again. Immunity wanes over time, with the steepest declines among people without so-called "hybrid" immunity from both an infection and vaccination.
Experts also now know that the risk posed by the virus to each person depends in part on their unique combination of previous vaccinations and infecting variants, the CDC told a panel of its outside vaccine advisers at a meeting late last month.
About 17% of COVID hospitalizations by the end of last year were from reinfections, according to a CDC study spanning data from 18 health departments.
Increasing seroprevalence has also changed how vaccine effectiveness is measured.
"It's become very difficult to measure prior infection in vaccine effectiveness studies. So if you think about the typical person being hospitalized that's picked up in one of these studies, they may have had half a dozen prior infections that they did a nasal swab at home and were never reported," the CDC's Ruth Link-Gelles said at the meeting.
Link-Gelles said vaccine effectiveness studies should now be interpreted "in the context" of most Americans already having previous antibodies for the virus.
This means researchers are now focused on measuring how much additional protection each year's new COVID booster shots will offer everybody, regardless of whether they got all their previous shots.