'Everybody Should See This Pain': On The Frontlines With ICU Nurses In Jackson Memorial Hospital's COVID Unit
MIAMI (CBSMiami) – In a special Facing South Florida with Jim DeFede segment, we heard directly from ICU nurses in the Jackson Memorial Hospital COVID unit. They gave an unprecedented look at what life is really like for health workers on the front lines. They shared their fears, their anguish and their pain.
The documentary-style report reveals an important part of the pandemic story that is often overlooked.
It all starts with Daphne, who spoke candidly to the camera and to her co-workers as she held the camera.
"My shift is over. First shift of three and honestly, last night wasn't too bad, but you know, it's a new bad now since COVID is around," Daphne said into the camera.
Daphne Stewart is an ICU nurse at JMH. Daphne now ends each 12 hour shift alone in her car, offering the same solemn prayer.
"Thank you Dear God."
She's grateful her shift is over. Grateful she is safe, and on this day, at least grateful no one died in her unit. That's not always the case. Nearly 500 COVID patients have died at Jackson Health System since the pandemic began. Doctors and nurses are not immune. Among the first victims of the virus was one of their own, longtime Jackson nurse Araceli Buendia Ilagan.
"It's just a different vibe in the hospital, in the atmosphere. I don't know. Just a different vibe," said Daphne.
Since the first COVID patients started showing up a Jackson five months ago, there is a grim sense of resolve for those on the front lines. You can see it on their faces, a stoicism that comes with not knowing when all of this will end.
"I'm here ready to start my shift," said Daphne.
To better understand their struggles, CBS4 News asked Daphne to document parts of her day and pose a few questions to her fellow nurses.
"You do know that this might be broadcast on TV and the internet?" she asked her co-worker Marta.
"I hope it is so you can see the real pain that a normal person or a real person is going through. You can see the exhaustion; you can see the emotional strain it's putting on everybody. If I'm straining and my family suffering, everybody should see this pain," said Marta.
What Daphne captured was unexpected, especially pictures of those on the frontline that reveal so much; the long hours, the helplessness of watching this virus take young and old alike and the doubts about whether their job is placing their own families at risk.
Daphne took her camera into the COVID unit where they all wear caps, goggles, and N-95 masks. It's where they keep the COVID patients behind a zippered layered of plastic protective sheeting.
Since the beginning of March, nearly 8,000 COVID patients have been admitted to Jackson Health System. Daphne recalls those early days
"My first COVID patient that I took care of I'll never forget him. I'll never forget that incident. I had to float to another floor. And within four hours, the guy, he was about 45 years old and he was dead. It was just him and I in the room."
Because visitors are not allowed in the hospital, it is almost always a nurse who is there with them when they die.
"I've been a trauma nurse for many years, and I've taken care of all kinds of catastrophic cases," said Marta. "And the most memorable, I will admit is a COVID patient I took care. She was an elderly patient and for some reason, just watching, just watching this patient, suffocate literally to death, and not being able to have any curable or anything to just ease her pain. There's nothing you can get for pain. There's nothing you can do for oxygen. There's nothing you can do. But just watch them just dwindle away is the most horrific memory I'll carry with me forever."
Carmen will never forget either.
"I was one of the first like on from our unit to float to a COVID floor. Both of my patients were violently ill. They were so sick that they're the kind of patients on this unit that we single. They were paralyzed. One of them was being prone multiple pressors each. He also needed fentanyl, propofol and ketamine because sedating him was an issue. So I mean, they were really sick. And the scariest part for me was the fact that I couldn't see them because central six is not an ICU. They're like regular rooms. And there's no window in the door. And there's no monitor outside. No camera. No nothing. When I close that door, I have no idea what's going on with those patients. I can't see the monitor. I can't see the patient and I'm my anxiety was through the roof for an entire 12 hours. I mean, at one point I actually cried in the bathroom from how frightened I was," recalled Carmen.
Five months into the pandemic, a rhythm forms, even as the number of patients increase. As an institution, Jackson has shown an amazing ability to process suffering.
"It's getting easier, but it's still not easy. We're still battling this, you know, people out in the streets are still not protecting themselves. They're still not wearing masks. And they think that this is not real. And they're focused on the numbers of how many new numbers and I want them to focus on the deaths, because they're saying now that they're making up all these numbers, right, it's okay, they're making them up. But I come here and I'm focused, one death is enough. One death is too many. You're going to call a family member. You're going to tell them. I don't want to be the one to do it. I don't," said Zenia.
Lest we forget, they have their own families to worry about.
"I have had moments where I stay away from home, just to be safe, weeks at a time," said Marta.
"Both of my parents, for example, are like, when are we going to see you? When are we going to see you? But considering that my parents are older, my dad is like, a sickly one. So I kind of refrain and I explained to him, listen, this is not the perfect time for me to you see because you just don't know," said Manoucheca.
"My mom is 86 and my dad is 89 years old. And it's just really taking a toll on the me," said Daphne. "Think about it. We've been dealing with this since March."
Marta's mother is also sick.
"I have an ill mom that I have not been able to see in about six months. And I'm really scared for her. And my heartbreaks, because I can't see my mother and her heartbreaks too because she can't see me and my heartbreaks because I don't know if I have much more time with her."
"I feel like I'm choosing the job over my parents, the patients over my family," said Daphne.
The fear for some is palpable.
Ashley, for instance, has a young child at home. She doesn't take off her PPE for her entire shift.
"I don't. I know people that feel safe and they do, but that's not how I feel. If I need to get something to drink and eat and take my few minutes I go to my car, I'm able to take off my equipment and get some fresh air, get a quick bite, whether it's you know, sip of water and then back to work," explained Ashley.
Have you thought about quitting Daphne asked Marta?
"I love what I do. I am proud to say that I do what I do. And coming to work every day has been an extreme struggle," said Marta.
Manoucheca agreed. "I've thought about it and I'm like, 'Oh, well, maybe I should just you know, give up on just working.' But then reality strikes back and then why? Because number one I'm a nurse, I care."
Ashley wonders how many more years of this and is this her new normal.
"How long will I be with all this equipment? will be for one year or 2 years?"
None of them enjoy wearing the masks.
"I come home sometimes and my sinuses hurt. I get sinus headaches because of these masks," said Marta.
"I mean for me, one of the challenging things is keeping a mask on. Um, because I have my moments where I'm like, 'Oh, I need to breathe. I need to breathe'," explained Manoucheca.
"So the doctor and I are there working with the patient and we're both coughing, looking at each other and I go 'Don't you feel like you have COVID when you wear the mask?' You suffer the symptoms. You have them, you have an itchy throat, your nose starts to run, your eyes start to get really like you feel like it's a sore throat and difficult to breathe through," said Zenia.
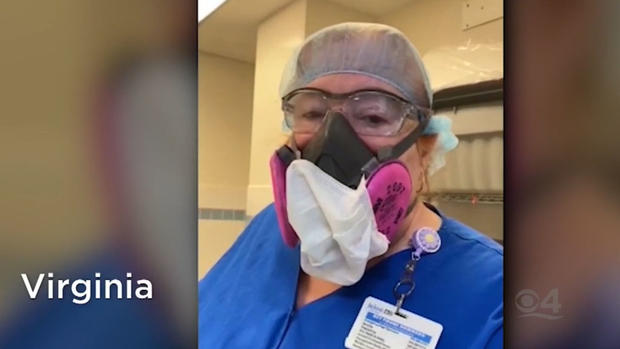
Virginia said the respirator masks are hot and hard to breathe through and showed Daphne the red lines on her face when she took off the respirator. She only had it on for 30 minutes.
Daphne asks her if her face hurts and she replies, "The bridge of my nose."
"It does take a toll on us mentally, and definitely physically, especially wearing the mask, we may have to do that. And we will hope that the community does that as well," said Felicia.
That sentiment is repeated time and time again. There's little patience for those who refuse to wear a mask.
"But I tell you one thing, if I can do it for nearly 11 hours out of the whole day, there is no reason why you should not be able to wear a mask for 20 to 30 minutes, wherever you're going. That's has a population of people that you need to social distancing. It makes no sense to me and if you can't do that, then you really need to think about the kind of person that you are and what you think of your fellow person. I really think you should," said Roberto.
At the end of her shift, Daphne ran into Ashley carrying her dirty clothes in a bag and asked her how she is feeling and how was her shift.
"It was a long, long day," replied Ashley.
Daphne won't be far behind. She'll be back in her car, offering prayerful thanks her shift is over.
CBS4 News and Jim DeFede thank Daphne and all the nurses who shared their experiences. And although the number of deaths in recent weeks have consistently set records in Florida, there is reason for some optimism as hospitalizations and Miami-Dade Dade and Broward have begun to drop. Experts believe it is because we began enforcing a mask mandate. Let's hope that trend continues.