Extreme heat is linked to pregnancy complications, including stillbirths and miscarriages — and the risk is growing
Our warming planet is putting those who are pregnant at higher risk — and the impacts go far beyond heat-related illnesses. Research shows that along with the dangers presented to the general population, extreme heat puts pregnant people — and their unborn fetuses — at risk of life-threatening conditions.
During pregnancy, expectant moms are more vulnerable to viruses and environmental conditions. And one of the threats comes from tiny insects: mosquitoes that can carry a handful of diseases.
Some of those diseases, like West Nile and eastern equine encephalitis (EEE) are rare but serious and can be deadly for the general population. Others, primarily found in tropical climates, like Oropouche virus disease, also known as "sloth fever," and Zika virus, can be particularly dangerous for those who are pregnant.
That danger will likely only expand going forward. Global temperatures are rising, largely driven by the overuse of fossil fuels that spew planet-warming emissions. And those rising temperatures are causing the typical mosquito season to last longer, extending the risk to vulnerable populations.
But this is just a mosquito-sized portion of a much larger threat that extreme heat poses to those who are pregnant.
"Climate change hurts women more," doctors at the Association of American Medical Colleges has as a headline on one of its website posts. "Extreme weather is linked to pregnancy complications, increased violence, and inescapable exposure to pollution and heat."
Here's why.
A bite risk for expecting parents
For those who are expecting, mosquito bites aren't just a nuisance — infections may pose a more serious threat to the fetus. Although these cases remain rare in the U.S., the CDC says West Nile, Zika and Oropouche viruses all pose a risk to those who are pregnant, with the latter two being more dangerous. West Nile, the leading cause of mosquito-borne disease in the continental U.S., can be transmitted to fetuses, although the risk is low, the CDC says, adding that there have only been a few cases of newborn infections.
Oropouche virus, otherwise known as "sloth fever," has been linked to stillbirth and birth defects, according to the CDC. There have been more than 8,000 cases of the Oropouche virus in Brazil, Bolivia, Peru, Colombia and Cuba reported so far this year, with at least 30 confirmed cases in Florida and one in New York, all of which have been linked to travel. The majority of global Oropouche cases are not in the U.S. Five cases of what's known as vertical transmission — the virus passing from mother to baby in utero — associated with fetal death or congenital abnormalities have been reported this year, according to the CDC, but none in the U.S.
Zika is also known to cause certain birth defects, but there have been no locally acquired cases of the virus in the U.S. since 2019. In 2015 and 2016, there were large outbreaks across Latin America.
According to scientists at the nonprofit Climate Central, "mosquitoes thrive in warm, humid weather" — conditions that become more common with climate change. The group looked at mosquito weather trends from 1979 to 2022 across 242 U.S. locations and found that 173 areas saw the number of annual mosquito days — where the average relative humidity is 42% or higher and daily minimum and maximum temperatures between 50-95 degrees Fahrenheit increase by more than two weeks on average. The South and Southeast U.S. see the most mosquito days, the scientists found.
With more mosquito days comes a greater risk of the spread of disease. While not all mosquitoes transmit diseases to humans — just about a dozen species in the U.S. do — more mosquito bites both here and abroad will increase the risk for more mosquito-borne infections, especially if Americans travel to areas where mosquito species that may carry infections like dengue and Oropouche.
Heat is deadly — even for the unborn
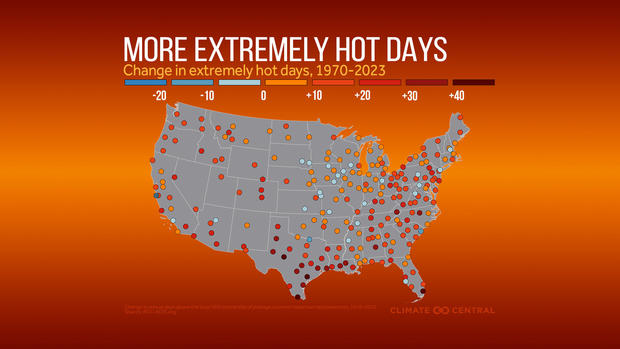
The world is already feeling the impact of climate change in a number of ways, with increasingly frequent temperature records, extreme storms, economic fallout and a wide range of health consequences.
The World Health Organization found that "preterm births — the leading cause of childhood deaths — spike during heatwaves." It also found that every 1 degree Celsius in minimum daily temperature over 23.9 degrees Celsius (75 degrees Fahrenheit), "has been shown to increase the risk of infant mortality by as much as 22.4%."
Dr. Anshu Banerjee, director of Maternal, Newborn, Child and Adolescent Health and Ageing at the World Health Organization, said the issue needs to be "urgently addressed."
"These studies show clearly that climate change is not a distant health threat, and that certain populations are already paying a high price," he said.
In their findings, experts found that high temperatures are linked to several adverse birth outcomes, including preterm and stillbirths. They also found that ambient air pollution — which can be exacerbated by high temperatures and wildfires — also poses a risk with an increased likelihood of high blood pressure, low birth weight and preterm birth. It can also have negative impacts on fetal brain and lung development, the WHO said.
Miscarriages, stillbirths and medical conditions rise with the heat
A 2020 systematic review of dozens of studies that looked at nearly 33 million births found a "statistically significant association" between heat, air pollution and adverse pregnancy outcomes, including preterm birth, low birth weight and stillbirth. Out of 58 studies, 84% found a "significant association between exposure to air pollutants and adverse birth outcomes," the researchers said. And nine out of 10 studies looking at heat conditions saw a significant association between exposure to heat during pregnancy and adverse outcomes.
Other studies have also found links between temperature and gestational diabetes and other pregnancy complications.
And hurricanes — a form of extreme weather made more frequent and intense by climate change — have been linked to an increased likelihood of complications, including fetal mortality.
Extreme heat can raise the toll of one of the leading causes of death of pregnant women — homicide
High temperatures aren't just an issue for medical conditions. Heat is also associated with a higher rate of violent crime and homicide — one of the leading causes of death of pregnant women in the U.S.
The Fourth National Climate Assessment said that "higher temperatures can lead to an increase in aggressive behaviors, including homicide." Numerous studies have shown how violent crimes, including murder, aggravated assault and rape, are all more likely when it's warmer outside. And for women, especially those who are pregnant, it can be particularly dangerous.
In 2022, Harvard researchers made it clear just how dangerous, with their finding that homicide is the leading cause of death for pregnant women in the U.S.
"Homicide deaths among pregnant women are more prevalent than deaths from hypertensive disorders, hemorrhage, or sepsis," researchers said. They cited one study that determined 68% of pregnancy-related homicides from 2009 to 2019 involved firearms. Black women face a "substantially higher risk" of being killed, they found.
A separate 2022 study found that pregnancy-associated homicide rose substantially when the COVID-19 pandemic began in 2020. That study found about 5.23 homicides in this category per 100,000 live births that year, with 80% of incidents involving firearms.
"The risk of homicide was 35% greater for pregnant and postpartum women than for their nonpregnant, nonpostpartum counterparts, who did not experience as large an increase from previous years," researchers said.
Lack of access to essential care
Getting access to care during pregnancy can already be difficult for many in the U.S. According to the CDC, about 4% of women did not have health care coverage at the time they gave birth in 2021. A study published that same year found that many women are not eligible for Medicaid before pregnancy or after 60 days postpartum, and that nearly 27% of new mothers with Medicaid-covered prenatal care were uninsured before pregnancy and about 22% became uninsured two to six months postpartum. More than 34% were not insured at either time.
After Roe v. Wade was overturned, it became even more complicated.
Associated Press data shows that the number of complaints of pregnant women being turned away from U.S. emergency rooms spiked in 2022 after the federal right to an abortion was stripped. Health care providers say that fear of prosecution or what could happen to their careers is contributing to the rise of complaints, which include a Texas woman who miscarried in an ER restroom after she said front desk staff refused to check her in. Another woman said she learned her fetus didn't have a heartbeat at a Florida hospital a day after a security guard turned her away.
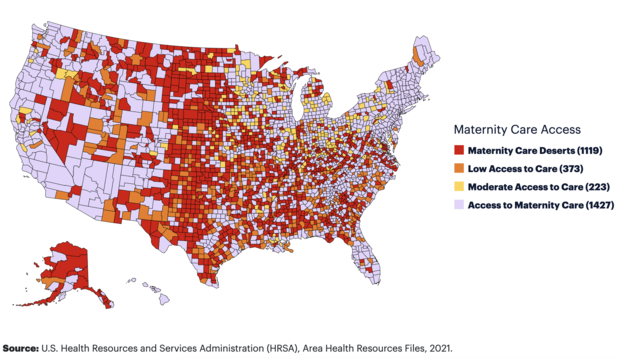
For many, proximity to care is also an issue. Last year, the nonprofit March of Dimes found that more than 2 million women of childbearing age are in "maternity care deserts," or areas that don't have nearby access to maternity care providers or facilities where they can give birth. Nearly a third of the U.S. counties fit this category, the group found. Two-thirds of maternity care deserts are in rural counties.
"The farther a woman travels to receive maternity care, the greater the risk of maternal morbidity and adverse outcomes," the report says. "...The distance a woman must travel to access care becomes a critical factor during pregnancy, at the time of birth, and in the case of emergencies."
Among those emergencies is extreme weather.
Tornadoes, hurricanes and floods — all of which have already broken disaster records in recent years — can quickly block access to medical care. Unsafe driving conditions and damaged infrastructure can block roads and make travel hazardous or impossible.
If someone is going into labor or is suffering a medical emergency, this lack of access can be fatal. And if they are able to make it to a medical facility, they still face the risk of the site itself losing power or being damaged, or not having enough staff resources with other emergent issues.
Climate change an "urgent women's health concern"
The American College of Obstetricians and Gynecologists put out a statement saying that "climate change is an urgent women's health concern and a major public health challenge."
"Environmental exposures, including those related to climate change, have a disproportionate effect on women's health and further exacerbate health inequities," the organization of health care professionals said, adding that it's "an urgent health care priority that affects everyone."
The group signaled that comprehensive climate, health care and infrastructure policy changes are needed to adequately address the issue, including curbing greenhouse gas emissions and more research into the impacts on women's health.