Medical conditions detected with a simple breath test
A growing body of research finds clues in your breath can reveal many things about your health. Doctors are using breathalyzer tests to diagnose a number of serious health conditions -- everything from gastrointestinal bugs to asthma -- and they may even hold promise for cancer. When it comes to your health, sometimes you shouldn't wait to exhale.
Click through to see what doctors can learn from a breath test.
Stomach cancer
Researchers have developed a new type of technology that may be the key to early detection for cancers of the gut. The technology, known as nanoarray spray, senses minute changes in levels of a specific compound in exhaled breath associated with stomach cancer.
A study published Monday in the journal Gut involved 484 people, 99 of whom had already been diagnosed with stomach cancer but had not yet started treatment. Researchers tested their breaths using gas chromatography-mass spectrometry (GCMS), an analytical method that identifies different substances in gas samples. The researchers then used nanoarray analysis combined with pattern recognition to analyze a second sample.
They found nanoarray sensing patterns could accurately distinguish between the different pre-cancerous stages to identify people who were at high risk for stomach cancer.
Currently, there is no effective noninvasive way to diagnose stomach cancer. This test could save lives by helping to detect the disease at a much earlier stage.
Next: A common food issue
Lactose and fructose intolerance
When doctors suspect a patient has an allergy to dairy, they may use a hydrogen breath test to reach a diagnosis.
Lactose intolerance means a person is unable to digest the sugars in milk. This allergy will result in a host of digestive problems including cramping, bloating, gas, or diarrhea any time the person consumes dairy products.
For the test, the patient drinks a beverage containing the equivalent amount of lactose found in a quart of milk, then breathes into balloon-like bags every 15 minutes for two hours. In this test, doctors are measuring the level of hydrogen in the breath. Breath normally contains a minimal amount of hydrogen but people with lactose intolerance will have levels that rise to 12 parts per million or higher. However, researchers say that the test doesn't work in everyone. Statistically, 20 percent of people with lactose intolerance don't actually exhale hydrogen.
Next: Blood sugar
Diabetes
A researcher in Massachusetts has developed a system that could allow diabetics to check their blood sugar levels by simply breathing. This not-yet-approved handheld device uses technology that was originally developed to detect chemicals in the atmosphere.
The test measures levels of acetone in the breath, which have been shown to correlate with blood sugar levels. Diabetics often have a condition known as ketoacidosis, in which the body produces large quantities of ketone bodies, the byproducts of the breakdown of fatty acids that contain acetone.
Next: Asthma
Asthma
Doctors use breathing tests to diagnose asthma and other pulmonary problems. In this instance, breath tests measure the volume of air a person is able to exhale, as well as how hard a person is able to breathe. A lower peak flow reading is a sign that lungs may not be operating at full capacity.
Some doctors may also use an exhaled nitric oxide (NO) test, which measures the level of NO in a patient's breath. A patient breathes into a mouthpiece of a machine to collect a sample of air. NO is a gas that's produced throughout the body, including the lungs, to fight inflammation and relax muscles. Higher than average levels of the gas can indicate that a patient's airways are inflamed, which could mean the person has asthma. This test can also help doctors determine if a steroid medication prescribed to a patient is actually working and if the asthma is under control.
Next: Helping the heart
Heart transplant
In 2004, the U.S. Food and Drug Administration approved Heartsbreath, a breath test meant to be used in tandem with a traditional heart (endomyocardial) biopsy on a heart transplant patient.
The test can help detect whether the person's body is rejecting the donor organ. Heartsbreath works by measuring the volume of methylated alkanes -- natural chemicals found in the breath and air -- in a patient's breath. The test detects certain markers that indicate oxidative stress, which may mean there is organ rejection.
Next: What's in your gut?
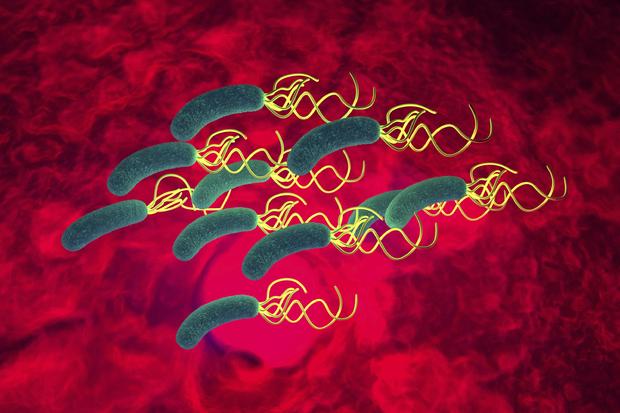
Helicobacter pylori
The urea breath test helps to detect the presence of H. pylori, a spiral bacteria that is responsible for most gastric and peptic ulcers and gastritis.
The test is effective because it measures the levels of carbon dioxide. H. pylori breaks down urea -- made of nitrogen and carbon -- and convert it into carbon dioxide. For the test, a patient swallows a capsule that contains urea. If carbon dioxide is detected when a patient exhales every 10 minutes, then doctors will know the bacteria has probably made a home in the gut.
Next: GI bacteria
Bacterial overgrowth syndrome
Small intestines bacteria overgrowth syndrome occurs when the bacteria typically found only in the colon proliferates in large quantities in the small intestines. This chronic problem leads to a number of gastrointestinal problems including diarrhea, constipation, irritable bowel syndrome, excess gas and bloating.
To diagnose a patient, a doctor may use a hydrogen breath test. A patient will drink a solution of sugar and breathe into a breathalyzer. If the bacteria happens to be fermenting in the small intestines it will be detected in the patient's breath.
Malaria
Malaria, which is spread by infected mosquitoes, is one of the biggest killers in the developing world. The World Health Organization estimates that in 2013 there were 198 million cases and 584,000 deaths, mostly among children under 5 years old.
Now researchers in Australia say they've developed a test that can diagnose malaria by detecting distinctive sulfur-containing chemical compounds in a patient's breath.
"What is exciting is that the increase in these chemicals were present at very early stages of infection, when many other methods would have been unable to detect the parasite in the body of people infected with malaria," Dr. Stephen Trowell, Research Group Leader at the Commonwealth Scientific and Industrial Research Organisation (CSIRO), said in a press statement.
Their study, published in the Journal of Infectious Diseases, was based on tests in a small number of volunteers. The researchers hope to develop inexpensive biosensor technology that could work in the field, providing an easier and more accurate alternative to blood tests in regions where malaria is endemic.