CDC warns of "alarming" rise of potentially deadly fungal threat in hospitals
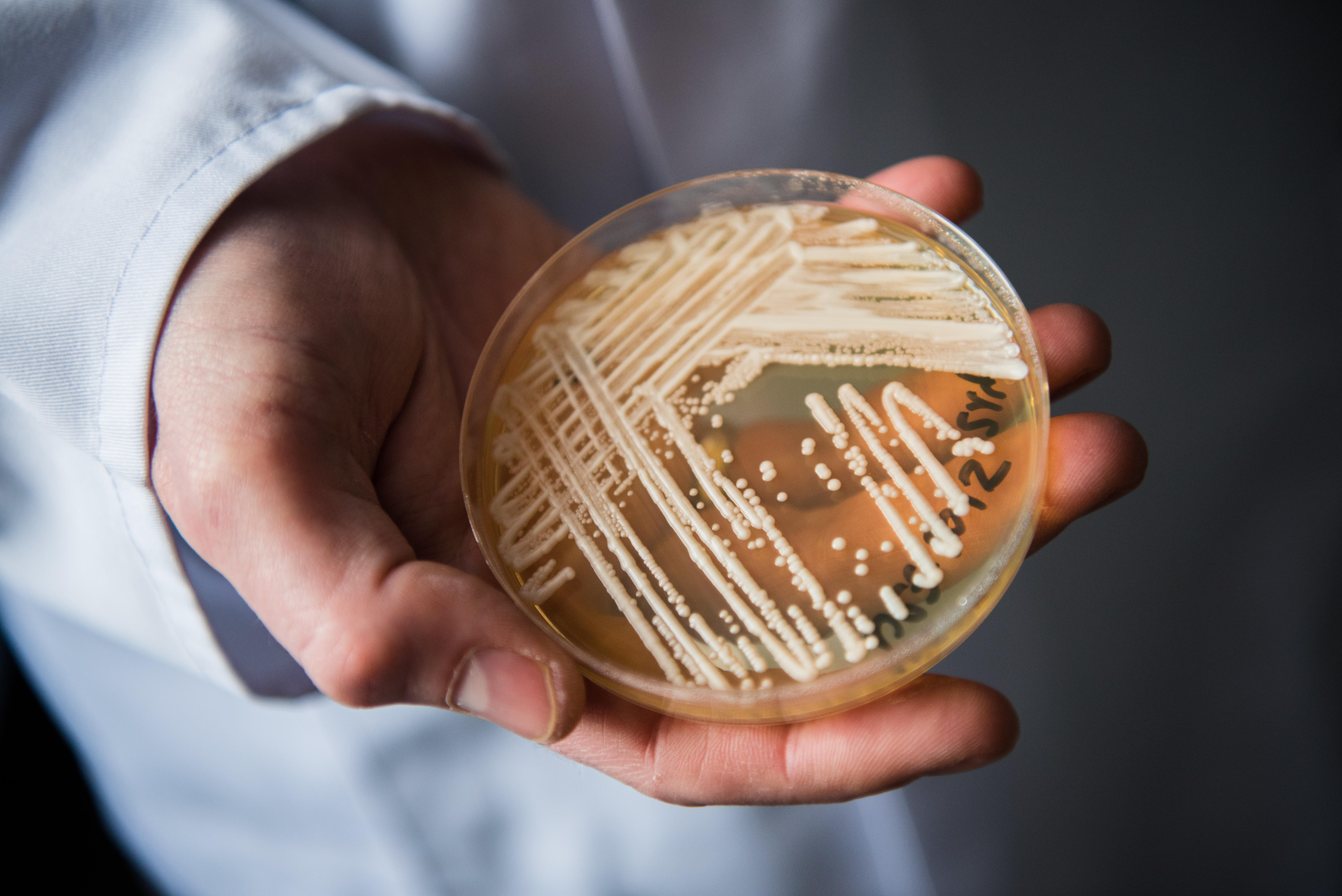
Cases of the drug-resistant fungus Candida auris are now climbing at an "alarming" rate in health care facilities around the country, the Centers for Disease Control and Prevention warned Monday, after reports of infected patients nearly doubled in 2021.
For several years after the first American cases were reported in 2016, only a few dozen Candida auris patients were reported to the CDC annually. But cases have begun to accelerate in recent years, according to the new CDC data published in the Annals of Internal Medicine.
By 2021, the annual tally of cases had increased 95%, from 756 in 2020 to 1,471 in 2021. Preliminary figures count at least another 2,377 cases for 2022. Thirty states and the District of Columbia have now reported Candida auris patients.
"We're continuing to see the number of cases increase. So what we saw before is continuing. It didn't stop. The issues that we've seen are continuing and it didn't resolve," says CDC epidemiologist Dr. Meghan Lyman, who was the report's lead author.
Candida auris is a form of yeast that often causes no symptoms on the body of healthy people. However, the fungus poses a serious threat to patients already weakened by other conditions, triggering serious and invasive complications as it spreads into the body's systems. Many cases have affected patients in hospitals and nursing homes.
Nearly all of the samples tested of Candida auris are already resistant to at least one class of antifungal drug. One in three patients with invasive infections die, although Lyman said it can often be tricky to assess the exact role the fungus played in some of these vulnerable patients.
Even in patients who survive invasive infections, some can remain "colonized" with Candida auris for years after they were treated.
"There's still a lot to learn about colonization patterns. But the treatment doesn't seem to completely— while it may treat the infection, we don't have evidence that it completely eliminates C. auris from their body," said Lyman.
Monday's report marks just the latest reminder of the growing threat posed by a range of drug-resistant pathogens.
A 2019 report by the CDC had already listed the fungus in the highest "urgent" threat tier among drug-resistant pathogens emerging around the country. In 2022, the CDC included Candida auris among the roster of drug-resistant infections that had grown at a worrying rate in COVID-19's wake.
Other countries have also reported new or accelerating Candida auris infections in recent years.
While it is tricky to measure the exact impact the pandemic has had on this trend, Lyman — who works in the agency's fungal diseases branch focused on drug resistance in health care settings — cited investigations that found some connections.
One CDC report investigated a 2020 outbreak in a COVID wing in a Florida hospital, after admission screening and some precautions were suspended during the pandemic.
"We continue to see challenges with infection control, so it's not all resolved now that COVID's not here. This is kind of a cautionary tale. But I think it highlights some things that may have been there before that got worse during COVID," said Lyman.
The World Health Organization last year ranked Candida auris as among the worst fungal threats facing public health today, given the danger it poses to vulnerable patients and the frustrations doctors face in treating and stopping drug-resistant outbreaks.
Nearly all tested samples of Candida auris are resistant to at least one of the classes of antifungal treatments, according to data from the CDC's network of antimicrobial-resistant labs.
Less than 5% of tested cases were resistant to echinocandin, the initial therapy recommended for treating patients battling Candida auris infections.
However, Lyman's report finds that cases of "pan-resistant" fungal infections — those with resistance to all available medications — have been inching up too. Health authorities reported outbreaks in 2021 in Texas and D.C. suggesting resistant infections are spreading, even in patients who never were treated with echinocandin.
Lyman said hospitals and nursing homes have ways of combating the spread of Candida auris, including by screening for cases and taking special steps to isolate infected patients.
"There's a lot of attention on the big outbreaks and widespread transmission but something that doesn't get as much attention are the facilities or areas that are able to prevent transmission," Lyman said.
Lyman says the ability of laboratories to detect and diagnose cases has improved over the years, as well as knowledge of strategies to curb transmission between patients.
"For some of these places, not ever seeing a case again may not be realistic. But there's still a lot that can be done to prevent spread," she said.