Q&A: Top Questions Answered About How The ACA Affects Massachusetts
The federal Affordable Care Act (ACA), signed into law March 2010, is modeled after the Massachusetts Health Care Reform law of 2006. Both laws require that most Americans have health insurance with a minimum level of coverage, and the laws provide assistance with premium costs for low-income households. The biggest change the ACA brings to the country is the requirement that states provide its residents access to the health insurance marketplace, where they can compare and purchase health plans.
Massachusetts is ahead of other states with the Massachusetts Health Connector exchange already well established. Most Massachusetts residents will see little change in their health insurance as provisions of the ACA take effect. The Massachusetts Department of Health and Human Services and the Massachusetts Health Connector authorities are working to reconcile differences between the federal and state laws so that Massachusetts will be in full compliance when the ACA exchanges open for enrollment October 1, 2013.
1. Will Massachusetts residents still purchase health plans through the Health Connector?
Massachusetts Health Connector will still be the website residents will access to compare and purchase health insurance. The Health Insurance Exchange/Integrated Eligibly System (HIX/IES) replaces the Virtual Gateway residents have used to access health plans. The new system allows Massachusetts residents to shop for health plans, apply for assistance and enroll in private and public plans with one application. In 2015, Phase II of the HIX/IES will allow residents to apply for public assistance programs such as SNAP and TANF through the exchange portal.
2. How will the ACA affect MassHealth (Medicaid), Commonwealth Care, and other Massachusetts subsidized health plans for low-income households?
Under the ACA, Medicaid eligibility is expanded to include households with incomes up to 133 percent of the Federal Poverty Level (FPL) with five percent of income disregarded, making the effective percent of FPL 138 percent. This expansion will make more residents eligible for the MassHealth program. A new MassHealth program, CarePlus, will offer coverage to non-elderly adults with incomes no greater than 133 percent of the FPL.
The Commonwealth Care and the Medical Security programs will be eliminated as many of its members will be eligible for MassHealth. Others with these plans that are not qualified for MassHealth may be eligible for federal tax subsidies to help pay for health insurance purchased through the Health Connector. Massachusetts will also offer subsidies, or a "state wrap," to bridge the gap between federal subsidies and premium costs to ensure Commonwealth Care members do not see their insurance costs increase.
3. How will income be measured for purposes of tax credits and subsidies?
The Massachusetts Health Reform law uses household gross income for determining eligibility for low-income programs. Under the ACA, residents will use their Modified Adjusted Gross Income to determine eligibility. In most cases, this will be a lower amount, opening these assistance programs to more residents.
4. Will residents still be able to purchase individual private policies through Commonwealth Choice?
The Commonwealth Choice program will continue to offer health plans that meet state and federal quality standards. The ACA will not affect residents that currently have a Commonwealth plan. Beginning in 2014, federal subsidies and tax credits will be available to help pay premium costs for people with incomes up to 400 percent of the FPL.
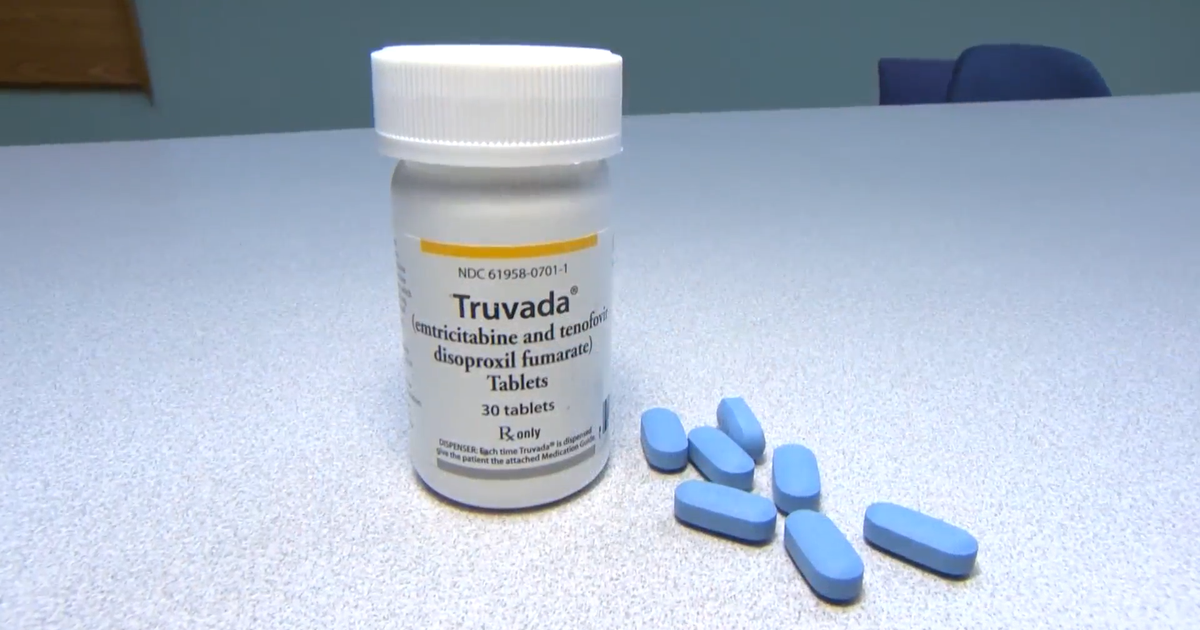
5. Will the ACA change the terms of health insurance policies purchased by Massachusetts residents?
Health insurance sold in Massachusetts through the Health Connector will continue to provide the core health benefits required by the state law. These benefits are similar to the essential health benefits required under the ACA. Additionally, the ACA requires that insurers cover preventative care such as wellness checkups, cancer screenings and vaccinations, with no co-pay or deductibles.
6. Will dental insurance be offered through Health Connector?
Pediatric dental benefits are required by the ACA and may be included in a health care package or offered as a standalone policy. Adult dental benefits were cut from the Massachusetts state budget in 2010. The 2013 budget partially restored these benefits, allowing coverage for care of front teeth. The 2014 budget further expands adult dental care to include fillings for all teeth.
7. What are the penalties for individuals that do not purchase health insurance?
Individuals who can afford health insurance but fail to purchase a plan, with a few exceptions, must pay a tax penalty under both Massachusetts and federal law. In Massachusetts, households with incomes up to 150 percent of the FPL are not required to pay a penalty for lack of coverage. For 2013, this amount is $16,764 for one person. The federal law has a lower income threshold, $10,000 for an individual.
Penalties in Massachusetts are assessed on a sliding scale, based on income above 150 percent of the FPL. For 2013, annual penalties begin at $240 and reach as high as $1,272. The ACA penalty for 2014 is $95 per adult and $47.50 per child up to $285 per family or one percent of family income, whichever is greater. Massachusetts legislators are expected to amend the state's law regarding penalties so that residents will not be paying both state and federal penalties in full.
8. Will adult children be able to stay on a parent's plan?
Health plans in Massachusetts must allow children to stay on their parents' plan until they reach age 26 or two years after losing dependency status, whichever comes first. The ACA expands this provision to include all children younger than 26 regardless of dependency status, even if the child no longer lives with his or her parents.
9. Will employers that do not offer their employees health benefit still be required to pay the Fair Share Contribution?
The Massachusetts law required employers with 11 or more employees make a minimum contribution to employees' insurance premiums or pay a Fair Share Contribution of up to $295 per employee. Governor Deval Patrick signed legislation repealing this provision effective July 1, 2013 in anticipation of the ACA employer mandate.
The federal mandate applies to businesses with 50 or more employees, and the penalty for not providing affordable health insurance can be as high as $3,000 times the number of full-time employees, excluding the first 30 employees.
Originally, the ACA employer mandate was to take effect January 2014, but the Obama administration has delayed enforcement of this provision until January 2015.
10. What assistance is offered small business owners who wish to offer employees health insurance benefits?
Beginning in 2010, businesses with 25 or fewer employees with annual average wages less than $50,000 each may qualify for federal tax credits of up to 35 percent of the employer's premium costs. In 2014, this tax credit increases to 50 percent when employee health plans are purchased through the Massachusetts Health Connector.
Gillian Burdett is a freelance writer covering all things home and living. Her work can be found on Examiner.com.